How conquering a rare leukemia in children revolutionized cancer care for millions
Behind the high cure rates for pediatric leukemia is an amazing story that transformed the whole field of cancer treatment and research.
Fifty years ago, children with an aggressive form of leukemia went from diagnosis to death in a few months, as the disease rampaged through their lymph nodes, spleens, livers, and nervous systems.
Today, 90 percent of children with the blood malignancy, called acute lymphoblastic leukemia (ALL), are cured.
That success story — one with deep Philadelphia roots — is even more phenomenal than it sounds. While ALL accounts for almost a third of pediatric cancers, it is a rare cancer overall, with about 2,900 annual diagnoses in the United States. Yet this uncommon malignancy is the tie that binds giants of oncology research, scientific breakthroughs, revolutionary drugs, and startling philanthropy, not to mention a Pulitzer Prize-winning book that became an acclaimed PBS documentary series.
“The road to curing most children with ALL may be the greatest success story in the history of cancer,” declared an American Society of Hematology history article.
Last month, a new chapter was added. An expert consensus panel released the first international treatment guidelines for the disease, because most children are no longer being enrolled in clinical studies aimed at finding the best approaches.
In celebration of this inspiring story, here are some historical highlights.
The first effective therapy
Sidney Farber, for whom Boston’s Dana-Farber Cancer Institute is named, is considered the father of modern chemotherapy. Besides being a scientific innovator, he was a genius at advocacy and fund-raising, and his collaboration with notables including philanthropist Mary Lasker led to a quadrupling of the National Cancer Institute’s budget between 1957 and 1967.
But in the early 1940s, Farber was stymied. The young pathologist at Boston Children’s Hospital couldn’t find anything to help the kids dying on the leukemia ward.
He knew that studies during World War II had shown folic acid, an essential vitamin, could cure certain anemias that were caused by a deficiency of healthy red blood cells.
Farber theorized that folic acid might also treat leukemia, in which the bone marrow spews immature white blood cells, called lymphoblasts, that grow uncontrollably.
“He tried it in some children, and it failed and seemingly made them worse,” said the above-mentioned American Society of Hematology article.
Maybe, Farber reasoned, folic acid actually stimulated the bone marrow to make blasts. Maybe a folic acid blocker could curb this growth.
Coincidentally, the Lederle pharmaceutical company was testing the first folic acid antagonist, called aminopterin. It had dangerous side effects, but it worked as Farber hoped. After he gave the drug to 16 children in late 1947, 10 had dramatic but temporary improvements. The landmark study was published six months later in the New England Journal of Medicine.
The next breakthrough, in 1950, was the development of 6-MP (mercaptopurine) by Gertrude Elion and George Hitchings, who would go on to receive the Nobel Prize. The drug disrupted the DNA of fast-growing cancer cells and was effective not only against ALL, but also adult leukemias and ulcerative colitis. About the same time, inflammation-fighting corticosteroids such as methotrexate were introduced, further improving survival of children with ALL.
Still, the lymphoblasts eventually developed resistance, sending children back into a downward spiral.
Total therapy
In 1962, Danny Thomas — the Lebanese American comedian, singer, actor, and devout Catholic — made good on a promise to the patron saint of hopeless causes with the opening of St. Jude Children’s Research Hospital in Memphis. To this day, the hospital boasts that “families never receive a bill for treatment, travel, housing, or food.”
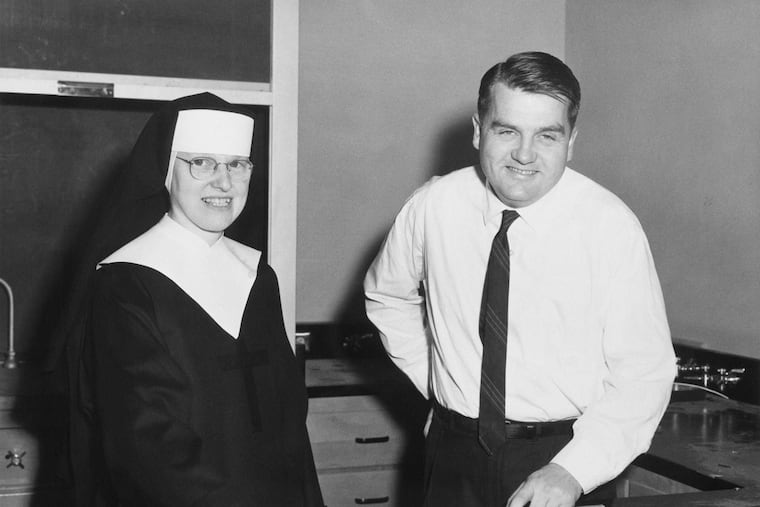
For the hospital’s first CEO and director, Thomas tapped Donald Pinkel, an oncologist focused on curing ALL.
Pinkel and his colleagues identified four major obstacles to that goal: drug resistance, drug toxicity, central nervous system relapse, and, most of all, the pessimism of doctors who assumed ALL was unbeatable, according to a St. Jude history article.
Pinkel’s team collaborated with other medical centers to conduct groundbreaking clinical trials of a regimen involving multiple drugs and radiation. Called “Total Therapy,” it is the backbone of the current intensive treatment protocol, which typically consists of three years of chemotherapy divided into four parts: inducing remission; wiping out undetectable disease; preventing relapse with maintenance drugs; and eradicating cancer hiding in the central nervous system.
By the late 1960s, Total Therapy was curing half of the children who got through it.
Last month, Pinkel, now 92, received the Giants of Cancer Care award — the latest in his long list of prizes and honors — from OncLive, the website of numerous publications for oncology professionals.
Targeted therapy
Despite huge progress, a subset of ALL children continued to have a grim prognosis with standard chemotherapy. Their disease was driven by a genetic defect that has become a landmark in medicine: the Philadelphia chromosome.
It was co-discovered in 1959 by David Hungerford of Fox Chase Cancer Center and Peter Nowell of the University of Pennsylvania.
When the two scientists “peered through a microscope and saw the stub of genetic material that would come to be known as the Philadelphia chromosome, they could not have foreseen … a chain reaction that would eventually enable the development of targeted and personalized cancer treatments,” says a Penn Medicine tribute article.
The identification of this abnormally short chromosome laid the foundation for the development of “tyrosine kinase inhibitors,” a class of drugs that interferes with cell growth signals. The first in the class was Gleevec (imatinib). It was initially approved for an adult leukemia but expanded to ALL in 2013. The National Cancer Institute says, without exaggeration, that Gleevec “transformed leukemia treatment and cancer research.”
With tyrosine kinase inhibitors, about 70 percent of children with Philadelphia chromosome-positive ALL are cured.
What’s more, a focus of the latest ALL research is identifying the genetic drivers of each child’s disease, then tailoring the intensity of treatment to minimize toxicity.
One result is that radiation to the head is rarely used anymore. In the past, it left many children with cognitive and skull damage, said Johns Hopkins University pediatric oncologist Patrick Brown, an author of the international treatment guidelines published last month by the National Comprehensive Cancer Network.
Immunotherapy
In April 2012, 6-year-old Emily Whitehead of Philipsburg, Pa., was admitted to Children’s Hospital of Philadelphia (CHOP). She was days from death. She had relapsed twice in the two years following her ALL diagnosis, despite relentless rounds of chemotherapy. She was too sick for a last-resort stem-cell transplant, in which blood cells that give rise to the immune system are wiped out and replaced with a donor’s cells.
Emily’s only hope was an experimental therapy made by genetically engineering her own disease-fighting T cells to attack her cancerous cells. Built on 20 years of research led by the University of Pennsylvania’s Carl June, the novel therapy had been tried previously only in six adults with blood cancers different than ALL; two experienced dramatic remissions.
The first-ever pediatric case did not go smoothly. The engineered T cells triggered a catastrophic immune overreaction, sending Emily into organ failure. In desperation, her doctors gave her a then-new immune-moderating drug. It saved her and became a vital part of the immunotherapy protocol.
Eight days after Emily regained consciousness. CHOP oncologist Stephan Grupp said tests showed her cancer was gone.
Five years later, the world’s first T-cell therapy, made by Novartis and called Kymriah, was approved for ALL. The following year, it was approved for a form of adult lymphoma — right behind Gilead Science’s T-cell therapy, Yescarta, for the same lymphoma.
Emily, now 14, marked seven years cancer-free in May. Her forever-grateful parents, Tom and Kari, raise money to support pediatric cancer research through a foundation set up in her name.
The Whiteheads and other stars of the ALL success story — including Farber, Lasker, Pinkel, June, and Grupp — were featured in Ken Burns’ three-part documentary Emperor of All Maladies. The 2015 film series was based on the Pulitzer Prize-winning “biography of cancer” by Siddhartha Mukherjee.
Mukherjee closes the series with an epigram, one that also sums up the ALL triumph: “If the cancer cell is evolving, then so are we.”