More than two years into the pandemic, hospital care still may not save you from dying of COVID-19
New figures from Pennsylvania and the U.S. show a continued death toll from COVID.
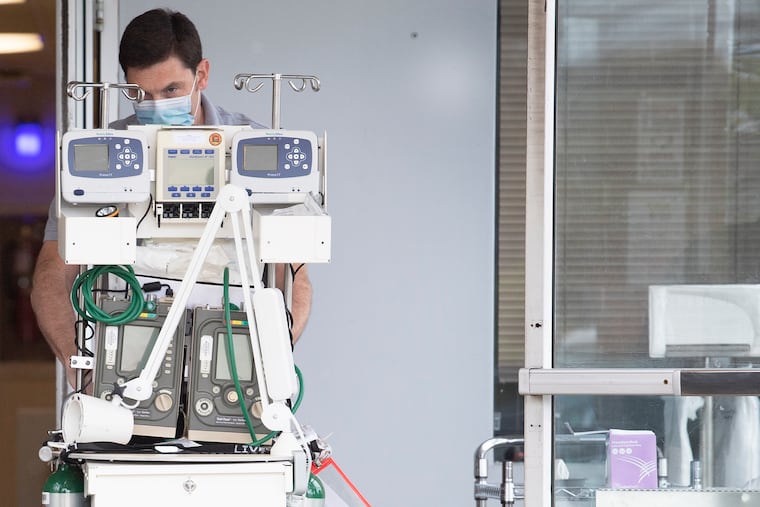
By the fall of 2020, the pandemic’s first year, doctors treating hospitalized COVID-19 patients said they were starting to get the regimen down to a science. They learned when to put patients on ventilators, administer steroids, and deploy an expanding array of newer drugs.
Yet the latest data from Pennsylvania and the U.S. show that as late as December 2021, one in seven people in the hospital with COVID were still dying — a rate not much better than at the start.
Experts say that comparing in-hospital death rates from then and now is not necessarily appropriate, in part because the data do not indicate the patients’ other health conditions, or whether, once the vaccines were available, they had gotten the shots. But the numbers are nevertheless a reminder that even now, a steady stream of people are going to the hospital with COVID, and plenty are so sick that they won’t survive.
Improvements in outpatient therapy have prompted some physicians to change their thinking on whom to admit to the hospital, said Lewis J. Kaplan, a professor at the University of Pennsylvania’s Perelman School of Medicine.
“These days, if you get admitted the hospital because of COVID,” he said, “you’re generally really sick.”
The state data, from the Pennsylvania Health Care Cost Containment Council, also reveal a trend that has changed little since the start: Older patients with COVID are more likely to need to go to the hospital — and once there, are more likely to die. Between March and June of 2020, the agency’s figures show that 28.2% of people over 85 years old who ended up in the hospital died there. By the end of 2021, that mortality rate had declined to a still-sobering 20%.
The U.S. data, taken from 59 hospitals by the CDC’s National Center for Health Statistics, are not broken down by age. But generally, the people now being hospitalized with COVID either have underlying health conditions, or have not been vaccinated, or both, said Kaplan, who served as president of the Society of Critical Care Medicine during the pandemic’s chaotic first year.
Both the Pennsylvania and U.S. figures stop at the end of 2021, when the omicron surge was getting underway. Cases and hospitalizations declined sharply by the spring of this year, yet lately they have risen once again. And the death rate, while low by the standards of the pandemic, persists at nearly 500 deaths per day.
If current trends continue, 39,000 people could die of COVID from July 11 to Nov. 1, according to the latest model from the Institute for Health Metrics and Evaluation (IHME), a research center at the University of Washington.
And many of those deaths will occur in the hospital, even with the latest treatments, IHME research scientist Sarah Wulf Hanson said.
Like Kaplan, she cautioned against reading too much into the trends in hospital mortality rates, as both the Pennsylvania and U.S. data include patients with “incidental” cases of COVID — that is, another medical condition was the primary reason for admission.
Studies suggest mortality rates also can rise as the result of hospital crowding during pandemic surges, as hospitals scramble to stretch their resources, she said.
» READ MORE: COVID vaccine caused early tension at Moderna, new book says
Yet the continued death toll is a clear sign that better treatments are still needed, Hanson and Kaplan agreed. And even those who survive still can experience long-term disability.
Along with improvements in care, Kaplan called for continued precautions outside the hospital.
It’s no secret that most people stopped wearing masks long ago, but the face coverings and other precautions remain important in certain situations, he said. Healthy 30-year-olds may have little to fear from COVID these days, especially if they are vaccinated. But they can still pass it on to others at greater risk.
“That simple message: take care of one another. It’s a social relationship that I think we need to recover,” he said. “In high-risk places, look after the people who are vulnerable.”