70% of imported KN95 masks fail U.S. filtration standards, study finds
For the study, researchers looked at nearly 200 KN95 masks from 15 manufacturers, including models purchased by some of the country’s largest health systems.
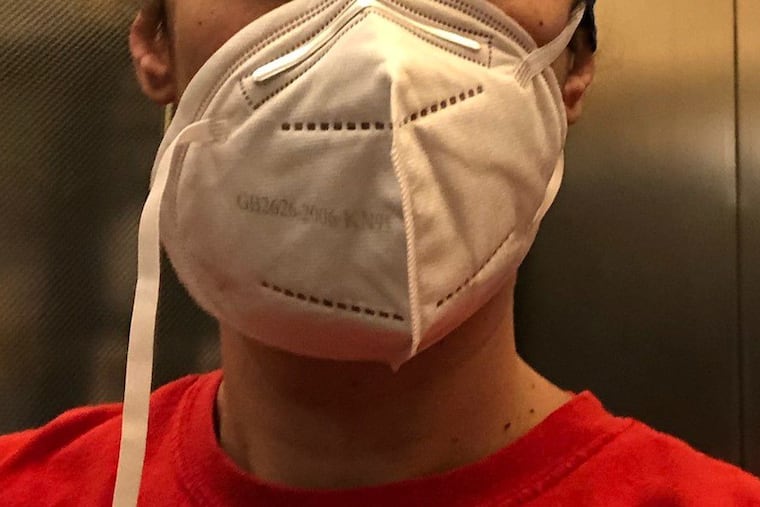
Up to 70% of KN95 masks do not meet the U.S. standards for effectiveness, according to a new study by ECRI, a Pennsylvania-based patient safety organization.
The findings suggest an increased risk of contracting COVID-19 for health-care workers and patients at hospitals that imported the masks from China to deal with massive shortages of protective equipment during the early days of the pandemic. (N95 masks meet the U.S. standards for effectiveness.)
Public health experts have already criticized KN95 masks for featuring ear loops instead of straps that go around the head and neck. This feature prevents the mask from sealing effectively against the wearer’s face, experts say.
ECRI researchers looked at nearly 200 KN95 masks from 15 manufacturers, including models purchased by some of the country’s largest health-care systems, and found that from 60% to 70% of the imported masks do not filter 95% of aerosol particles. They tested the masks by attaching them to a machine, which then blew particles at the mask. Researchers then counted the particles that were found on the inner portion of the mask.
“We started to test the masks to help our members and clients,” said Marcus Schabacker, ECRI’s president and CEO. “We were really stunned by the results. The most stunning thing was that we would test masks from the same manufacturer, and some would pass, while some wouldn’t. These masks were claiming on paper to filter out 95% of particles, but they didn’t. That was reason enough to raise the alarm.”
Health-care systems ordered hundreds of thousands of KN95 masks after the U.S. Food and Drug Administration issued an emergency use authorization in April for masks that are manufactured in China to help hospitals cope with the shortage of personal protective equipment. The masks do not need to be approved by the National Institutes of Occupational Safety and Health.
Although there has been a recent increase in PPE production supported by the federal government, hospitals continue to report shortages. Schabacker said that hospitals should consider classifying employee risk to cope with ongoing shortages.
“Use high-value protectives in areas where they’re needed the most, like taking swabs from suspected COVID patients, doing an intubation or airway manipulation,” he said. “Secondly, we provide strategies on our resource center on extended use and safe reuse of masks.”
Researchers said that as long as the KN95s that don’t meet safety standards aren’t being used in situations where there are bodily fluids, they can still provide more protection than cloth or surgical masks.
“KN95s are not useless,” Schabacker said. “We still believe they’re better than standard surgical masks, so there’s no need to throw them out. Just don’t use them in high-risk areas.”