Anthony Fauci and unlocking the biggest mystery in medicine
Doctors are on the front lines of long COVID, affected between 1 and 2 million people in the U.S. Here's what's been learned so far.
They come to my office every week, sometimes every day. One is a college professor trying to make tenure but can’t teach because their heart rate jumps to 160 upon standing. Another is a nurse who is plagued by fatigue and cannot get through the grueling 12-hour shifts. A third has such profound fatigue they run their business from bed; they blur out the background on the zoom meetings and prop their head up with a hand.
These three, and many others, have been diagnosed with myalgic encephalitis, also known as chronic fatigue syndrome. The CDC recommends three criteria for diagnosis: a greatly lower ability to do activities that lasts six months or longer, worsening of symptoms after physical activity, and sleep issues that may include feeling weary after a full night’s sleep. Other symptoms may include cognitive dysfunction (“brain fog”), chronic pain, and light-headedness or dizziness when standing.
There are between 1 and 2 million with this affliction in America today, and with the ongoing COVID crisis, the ranks of the afflicted threaten to grow by many more millions. The layers of their life often strip away like paint, and a first casualty is often their job and whatever worth they got from it. If they are lucky, they have the assistance of a family. If unlucky, they battle in solitude.
As doctors, we often tell them to fight, to struggle. Walk 10 minutes a day and next week you will be able to walk 20. Two-pound weight exercises will turn into five pounds. We will cheerlead you out of this illness. Often, though, this approach only makes things worse, and the standby of graded and increasing movement will improve function does not apply.
The patients I see in my lung clinic, though, afford us a rare opportunity. Prior to COVID, it was thought perhaps a viral illness triggered this cascade of decline and misery. The usual suspects are Epstein-Barr virus or its cousin cytomegalovirus. They are only suspects, though. Now with COVID-19 we believe we have detained an offender.
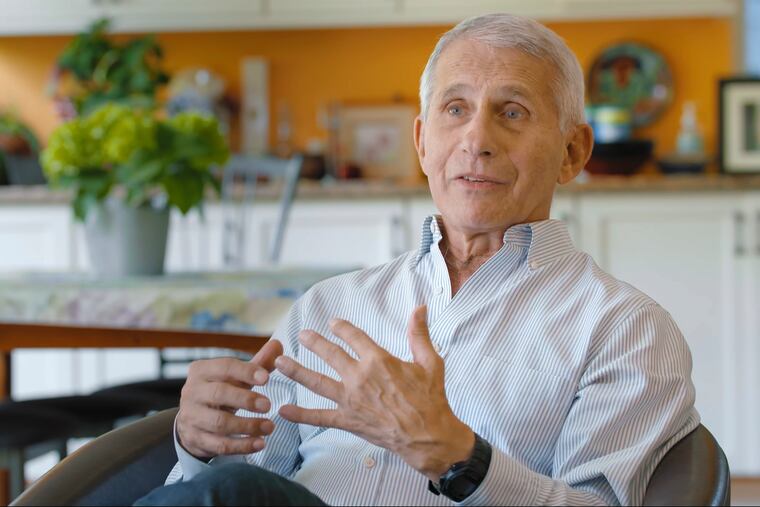
Former chief medical advisor to the president, Anthony Fauci is one doctor who sees the opportunity here. I spoke with him, and in his precise, careful fashion, he laid out a road map for how to approach ME/CFS.
First, stick with only post-COVID patients; do not dilute your sample with other post-viral conditions.
Second, make sure you have a very strict and agreed-upon definition of what long COVID constitutes: symptoms must be there for at least six months, and a level of significant disability must be documented.
Once you have your population, then cast a wide net into possible avenues of dysregulation. What blood markers were elevated at the start of their infection? What blood markers continue to be elevated after six months? Is there evidence of ongoing reaction to live or broken-down viral DNA? Who are the people who eventually get better? Who are the ones who continue to struggle?
Interesting data is being generated. One study in the journal Nature showed that patients who had died from COVID had clear evidence of viral substrate in tissues throughout the body, including the heart, intestine, and adrenal gland. Most damningly, the brain was frequently involved, with one patient having evidence of viral particles in their central nervous system a full 230 days after initial symptoms.
Another study from Yale shows that despite adequate heart and lung function, oxygen was not being utilized by muscles during exercise, pointing to mitochondrial dysfunction. A recent study out of the University of Pennsylvania implicated low levels of the neurotransmitter serotonin. No organ should be beyond analysis, beyond suspicion.
Large treatment trials have also begun, including interventions involving stem cells, exercise regimens, antibody infusions, and antidepressants like lithium and fluvoxamine. To date, however, there are no FDA approved medications for long COVID or ME/CFS. The mystery endures.
With COVID numbers recently rising, our sample size of people with long-term issues will continue to rise. The best protection against this is to avoid the disease if possible: hand washing, masks in high-risk situations, staying home if ill. Vaccines and boosters are very helpful, and recent studies have shown in both children and adults the vaccine significantly lowers the incidence of long COVID.
Suffering can be endured if there is the possibility of an end, if there is an expectation of convalescence, of the possibility of a return to a remembered life that was more productive, more engaged. We call this hope. With COVID-19 and the clinical trials going on, there is hope for the first time for the millions struggling under the crushing yoke of ME/CFS.
Michael J. Stephen M.D. is a Penn Medicine pulmonary physician and author of “Breath Taking, A Biography of the Lungs.”