A cardiologist on when heart surgery and stents can mean longer life
Sorry, but the study results do not mean that taking a statin for cholesterol and coronary blockages is just as good as an operation. You still need lifestyle changes.
Sometimes in medicine it takes a while to get things right.
It can be years before the result of a new study gains acceptance in the medical community. This may be from multiple causes, including faith in current treatment, concern that new findings don’t reflect real life, arrogance, and financial pressure from the medical-industrial complex.
Sometimes change happens fast.
In the early 2000s, a drug called Natrecor was used extensively to treat acute episodes of congestive heart failure, so-called fluid on the lungs. A subsequent study was published in the New England Journal of Medicine showing that Natrecor was no better than placebo, and its use quickly vanished.
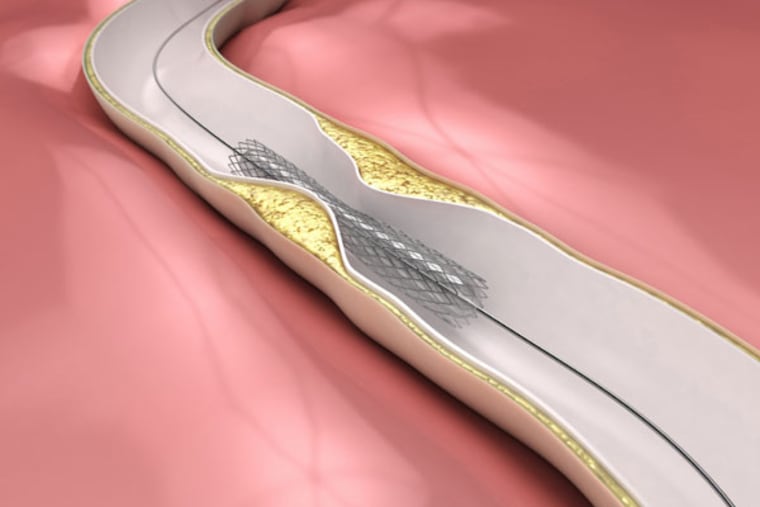
One of the enduring myths about heart disease is that elective bypass surgery or stenting for stable angina means longer life than just getting excellent medical care without surgery. Despite multiple trials that have shown no difference in the two approaches, there are hundreds of thousands of such operations performed every year. Studies that are older (COURAGE) and newer (ORBITA) have shown little difference between the treatments.
There is an important distinction: Stable angina is a gradual buildup of blockages in the coronary arteries. Unstable angina is when a plaque has either ruptured or cracked, or when the heart is at great risk for impending infarction (tissue death due to lack of blood supply). When angina is unstable, surgery with bypass or a stent performed soon after a heart attack is often a lifesaving measure.
A new trial has literally come to town, released Nov. 16 at the American Heart Association meetings in Philadelphia. This study is called ISCHEMIA, and it reaffirms the findings of earlier studies showing that coronary blockages, when stable, are treated just as well with the best of medications as they are with bypass surgery or coronary stents. It was a government-funded study, cutting down on industry bias, and conducted on more than 5,100 patients. It was led by researchers at NYU Langone Health and followed patients for more than three years, starting in 2012.
Cardiac death, heart attack, hospitalization for unstable angina, heart failure or cardiac arrest occurred in about 14% of patients in both the invasively treated group and the more conservatively treated group.
Here are the top take-home messages:
1. Bypass surgery or stenting will not help you live longer if you have stable angina than would the right medications, and making lifestyle changes
2. About 85% of participants in this study had a stent, 15% bypass, and used the latest technologies/techniques for treatment.
3. People who had significant chest discomfort (angina) or difficulty breathing did better after an operation or stent; it made symptoms better even if it did not prolong lives.
4. A separate arm of the ISCHEMIA study, which was directed toward people with kidney disease and angina, found the risk of death or heart attack to be high (more than 35%). There was no difference between the invasive or noninvasive groups, even if patients with kidney disease had angina.
5. In the ISCHEMIA trial, in the early months after surgery/stenting, there were more cardiac complications, but by four years, there was no difference with the non-invasive group. This was likely from the initial effects of invasive procedures.
6. The study results do not mean that taking a statin for cholesterol and coronary blockages is just as good as an operation. Although statins are important, they alone are not the answer. Weight loss, diet and exercise are at least as necessary.
7. Since in 2017, when the ORBITA study was first published in Lancet, it was estimated that 500,000 people received stents for stable angina every year, and the paper was “poised to shake up cardiology.” Not much has changed. Cardiologists continue to place stents and cardiac surgeons perform bypasses. I am hopeful that this new study will change the tide and we will see less invasive treatment in stable coronary artery disease.
David Becker is a frequent Inquirer contributor and a board-certified cardiologist with Chestnut Hill Temple Cardiology in Flourtown, Pa. He has been in practice for more than 25 years.