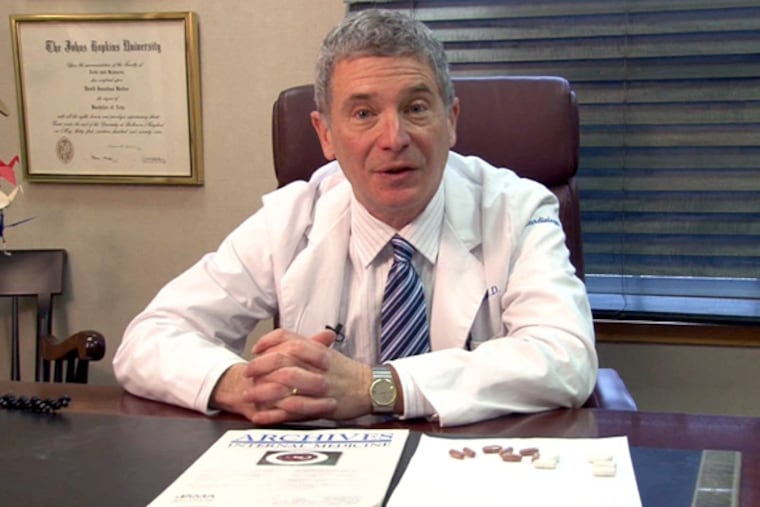
After brain cancer surgery, a physician gets an up-close view of rehab and what needs to change | Expert Opinion
For eight years, David Becker has written as a physician. This time, he writes as a patient.
I have written medical articles for The Inquirer for eight years. My goal has been to write medical columns that are easily understood by people who are not in the health professions. Knowledge is a potent ingredient for self-care, self-advocacy and healing.
Historically, my writing lens has been through the eyes of a physician. Today, I am changing lenses and writing though the eyes of a patient.
I was diagnosed with a malignant brain tumor just more than 2½ years ago. After responding well to treatment, I continued to live my life. In April, an MRI identified an asymptomatic reoccurrence. This rocked my world. The disease was back.
Surgery was recommended. I underwent two craniotomies over a three-day period at the Hospital of the University of Pennsylvania. The nursing and medical care was outstanding and encouraging to my recovery. Two days post-op, with my family by my side, I was walking 1½ miles a day in the hospital halls. The staff would high-five at each lap.
With optimism, I transferred to another hospital to begin my rehab.
» READ MORE: 5 questions: After a traumatic brain injury, she is helping other survivors
This was when my optimism began to wane. Although I had never fallen or slipped, upon admission, I was deemed a fall risk. I was placed in a locked ward and hooked up to alarm systems, my every movement restricted. No longer was I free to walk the halls. The alarms wailed every time I moved in the wrong direction. I was scolded and told to stay in bed for safety reasons.
Someone was required to watch me go to the bathroom and take a shower. It felt demeaning. I wish someone had warned me about the rules and limitations of this rehab unit.
My kids had jokingly labeled the place as “Brain Camp.” To me, it felt like “Brain Jail.”
I understand that patients with traumatic brain injury (TBI) are at high risk for falling and other safety issues. But not every patient with TBI is the same. In my field, cardiology, when a patient presents with congestive heart failure, different strategies are needed to treat symptoms and improve outcomes. Above all, every patient needs to be treated individually and with respect.
I believe that most people who enter the health-care field do so with a deep desire to help people heal. Yet, in my case, it felt as if other issues were driving my care. Could it be that the preoccupation with my fall risk was not only for safety, but also for safety metrics and insurance reimbursement? It’s interesting that when we were provided a list of rehabilitation facilities, the rate of falls was listed as a quality indicator.
» READ MORE: Humbled by a traumatic brain injury, Philly musician’s new mission is uniting people through jazz
If I were to fall and sustain an injury during my stay, the facility would be responsible for the cost. It turns out that insurance reimbursement also influenced the length of my stay.
Day 3 of rehab was a productive day. My wife attended all therapy sessions to learn what would be beneficial for me at home. At the end of the day, she said to the physical therapist (PT) that she would be back the next day after therapy. To our surprise, the PT said there were no more therapies ordered.
I was puzzled. Why would I need to spend another sleepless night in “Brain Jail” if there would be no further therapy? This seemed counterintuitive to my recovery. Getting a clear answer seemed impossible. They told us we needed medications delivered. It made no sense. Why not get them through the local drugstore?
Then one staff member quietly shared that insurance does not cover the day of discharge. That meant that the Day 3 therapies might not be reimbursed if I didn’t spend another night.
There is no question that the therapists should be paid. However, this payment should not come at the expense of what is best for the patient. We managed to get a discharge that day. My rehab experience took an emotional toll. I wonder what would have happened if I didn’t have medical knowledge and a fierce advocate (my wife — who also is a nurse) by my side.
Based on my experience, TBI rehabilitative care is in need of reassessment, reflection and improvement.
David Becker is a board-certified cardiologist with Chestnut Hill Temple Cardiology in Flourtown. He has been in practice for more than 25 years and is a frequent contributor to The Inquirer.