Cancer patients staring down ‘scanxiety’ | Expert Opinion
Family members of a physician and patient look back on his experiences and offer coping tips for others.
Our beloved husband, father, and longtime Philadelphia physician David Becker underwent about 28 brain scans in four years as he was diagnosed with glioblastoma and received treatment.
The week before an upcoming scan, David and each member of our family would feel symptoms like stomach butterflies, irritability, racing heart beats, poor concentration, and reclusiveness.
Turns out, we were experiencing “scanxiety,” as author and cancer survivor Bruce Feiler defines the distress and anxiety felt by patients and loved ones before, during, and after cancer-related imaging.
In April 2023, David shared his scanxiety experiences with Philadelphia Inquirer readers in his health column. We received an outpouring of responses from readers about how they coped with their own scanxiety. Many of their experiences aligned with emerging scientific understanding of how scanxiety impacts cancer patients.
For some readers, scanxiety was an aspect of their cancer journey that was never discussed. They explained it was easier to discuss physical health than mental health. We want them to know: Scanxiety is very real and it affects patients across the cancer continuum, no matter the diagnosis, the stage, or treatment. This emotional distress can vary from person to person and emerge at different times during testing and treatment.
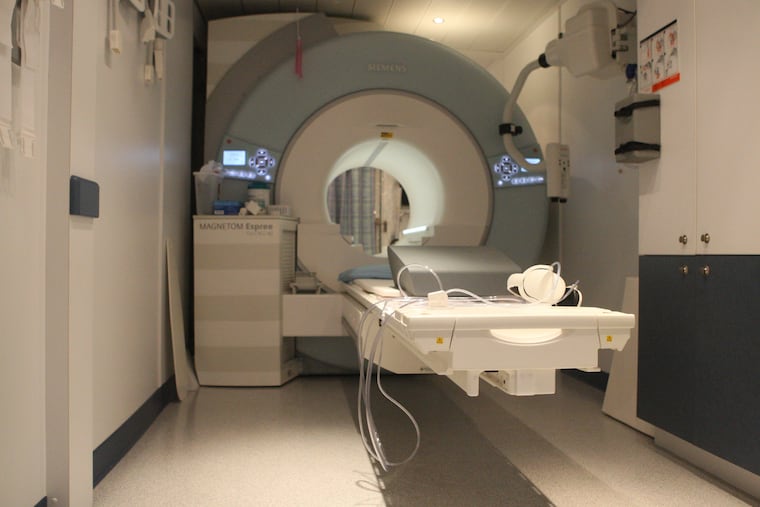
Scanxiety is so insidious because it is associated with uncertainty and fear about what test results will show. Cancer scans are high stakes. They identify disease progression, disease recurrence, and future treatments. Discomfort during imaging, such as claustrophobia, or fear that exposure to radiation will lead to other cancers can further exacerbate scanxiety.
Individuals with high levels of scanxiety are at risk for poorer quality of life, poorer emotional well-being, more difficulty sleeping, higher blood pressure, a fast heart rate, increased irritability, poor concentration, and lower motivation for daily activities. In some cases, scanxiety can lead patients to avoid scans altogether, which prevents them from getting the treatment they need.
Since it can be hard for patients to share their own anxiety, experts recommend that health-care providers screen for baseline anxiety and stress and use this information to identify additional scan-time supports for patients who are likely to benefit.
Scanxiety is worsened by the health system’s larger challenges. Many readers responded that a time of peak scanxiety was after the scan, as it could take up to a week or longer to see their oncologist to learn the results.
This time between the procedure and receiving results is often described as the most nerve wracking. Health-care providers could work to reduce wait times to lessen patient anxiety.
Some experts suggest releasing results to a patient portal, so that patients can receive the information sooner. But doing so is tricky, because medical jargon in the absence of expert interpretation can lead to patient confusion, misunderstanding, and increased anxiety.
For our family, awaiting scan results was the most anxiety-provoking period, and we are grateful to our health-care providers for their efforts to shorten how long we had to wait for results.
Insurance stress also compounds scanxiety. As one reader shared, “I thought how lucky you are to have the scans every two months. My husband’s doctor had to fight with the insurance company for his PET scans.” No one should have to use their limited emotional bandwidth to fight with their insurance company about coverage. Needed health-care reform won’t get rid of scanxiety, but could go a long way to reducing it.
Readers also shared strategies they used to cope with scanxiety, such as listening to music, meditating, talking to family members, or finding a support group. There is little data to suggest what may work best, but experts recommend all of these strategies and more.
We do know that social support is critical, because more isolation is associated with more distress. Ultimately, the best way to manage this stress is unique to each individual. Talking about scanxiety with health-care providers can help people to get support, whether it be therapy, medication, or more informal strategies.
And finally, the irony; As difficult as it is to deal with, patients want and need the scans. One reader reminded us, “having a “next scan” means you are still in the game.”
Oh, how we wish we were still in the game. David is no longer with us. He wrote his columns, hoping to simplify medical terminology and allow patients to feel connected and seen. We are trying to do the same here. If you or anyone you love struggles with scanxiety, let your doctor know that the scans are hard emotionally and ask what resources they can offer you to help you cope.
Sherri Becker has a doctorate in nursing and is an adjunct professor of Nursing at Gwynedd Mercy University. Emily Becker Haimes, PhD, is an assistant professor in the Center for Mental Health at the University of Pennsylvania. Chloe Becker, MD, is starting an internal medicine residency in Washington, D.C.