Medical student faces uphill battle on rethinking weight | Expert Opinion
Working with a size-inclusive physician has been eye opening for a third-year student, as some in the medical community seek to redirect conversations around appearance to conversations about health.
I opened the clinic schedule for the day, scanning down the list of 20-minute appointments. “Blood pressure check,” “annual physical exam,” and “rash” were some of the reasons listed for why the patient made the appointment. I hurriedly threw on my stethoscope, tripping over an electronic cord as I made my way into the first exam room.
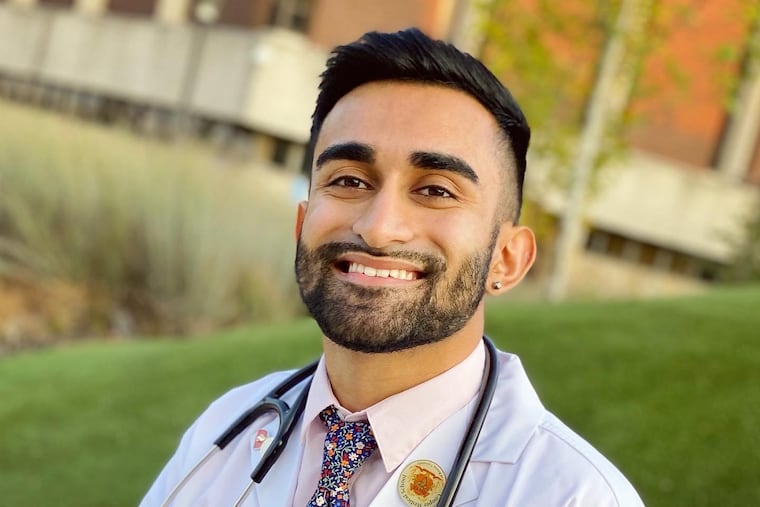
I recited my usual greeting, perfected over the past year as I did my third-year medical school clerkships. “My name is Milan Arya, I am a medical student working with the doctor today. Is it OK if I ask you a few questions before she joins us?” The patient nodded. “I see that you are here to talk about your blood pressure, correct?”
“Actually, I wanted to talk about how I could lose weight.” This patient response had become a familiar one. Over my week-long rotation in the primary care clinic, I witnessed how often patients put a conversation about weight on the agenda, regardless of what medical issue they made the appointment for.
Later in the day, I greeted another patient who had scheduled a follow-up visit after starting an antidepressant medication. She described being unhappy with her body image and believed she was gaining too much weight.
“Your labs here look completely normal. Increasing your exercise will overall improve your well-being, but I do not recommend using the number on the scale as a goal or a measure of your health,” I replied, hoping my words would address the patient’s concerns while redirecting their focus on their weight. My mentor, Mara Gordon, a size-inclusive physician at Cooper Medical School whose medical practice works to be neutral to weight as a factor in health, was pivotal in shaping my understanding of this topic.
I understood how my patients felt. Growing up in an Indian-American household, weight was a constant subject of discussion. My sister was teased by my family for snacking between meals or ordering one too many sugary iced coffees. The guilt that she carried manifested in highly disordered eating habits. For example, she would eat very little at mealtimes and would subsequently rummage through the fridge for food in the middle of the night. Her self-confidence was so wrought from the criticism that she wore face masks and hoodies in public at all times, thus shielding her body from the public eye.
“If only we could take some of the weight off of her body and put it on yours,” my family would often joke. I have always occupied a smaller body, which invited its own set of quips from my parents and extended family.
“Are you sure you’ve eaten enough?” They would ask me, as I felt the food rise in my throat and my abdomen distend from overeating. The portions handed to me would be unusually large and not finishing them would be a sign of disrespect. As the spotlight burned against my skin, I saw my sister increasingly recede into the shadows, trying best to stay hidden from their critical gaze. This is reality for many Indian households, where fat-shaming is unfortunately a common occurrence.
Our society has conflated weight as the inception of all ills. The messaging is loud and clear from the very moment we are born. The usage of BMI as a clinical tool is just one way in which we standardize differential treatment of people inhabiting larger bodies.
The reality is that research over the last 70 years has already shown that there is little correlation between an individual’s BMI and their metabolic health. An individual with a BMI of 24 may still have diabetes, high cholesterol or hypertension. There are so many other factors that determine health, such as diet, exercise, genetics, environment, income, housing, and inequality.
Healthiness comes in all shapes and sizes. I saw this when I interacted with a patient with a BMI of 29, who would be classified as ‘overweight’ but had perfect blood pressure and blood sugar levels.
It is not always possible to undo decades of societal conditioning in a 20-minute visit. Sometimes patients just want to lose weight, regardless of how healthy they might otherwise be. For instance, one patient described feeling like he could not climb the stairs of his apartment without getting winded. Another said that she just felt unattractive. I have learned that it is important to explore the reasons for why patients want to lose weight and what their weight loss goals are.
These are scenarios that UWorld (an online question bank utilized by students preparing for their medical licensing exams) did not prepare me for. As I take my first foray into the frenzy of primary care, many questions arise in my mind: Do I prescribe Ozempic for the patient whose blood sugar levels are just barely into the pre-diabetic range? Do I recommend bariatric surgery for the patient who suffers from treatment-resistant depression and needs a psychiatrist, not a surgeon?
“I am tired of feeling like this. I am tired of people looking at me and seeing my body before they see me,” one patient lamented, as I handed them a box of tissues. I am brought back to the dinner table, where my sister and I are on opposite ends at the front lines of war.
As I wave goodbye to my last patient of the day, I am filled with the doubts, insecurities, and hopes of the patients that I saw that week. My role as a medical student is a small one, but I am privileged to have the opportunity to cultivate a safe and affirming environment for patients entering the clinic. I hope to remind them that weight does not equate health and that they are worthy regardless of what the number on the scale reads. It is what my sister and I needed to hear growing up.
Milan Arya is a fourth-year medical student at Cooper Medical School in Camden with the goal of becoming a primary care physician.