Medical Mystery: When multiple physicians couldn’t help, he turned to the internet and a nurse practitioner
A specialized blood test requested by Larry Weller — not the half-dozen doctors he had seen — would reveal the reason for his inability to chew and swallow.
Beginning in the summer of 2016, Larry Weller, then 70, experienced bouts of laryngitis, even though he hadn’t had a respiratory infection. His family physician referred him to an ear, nose, and throat specialist who ramped up the dose of his acid-blocking medicine. Acid reflux can sometimes cause a hoarse voice. Weller, who lives in Bloomington, Ill., had been diagnosed with reflux years earlier and had taken medication that controlled the problem.
But after three months on a high dose of the drug, his hoarseness lingered.
“It didn’t change anything,” recalled Weller, a retired agronomist.
In October 2017, the ENT performed a videostroboscopy, a procedure that uses a scope to inspect the vocal cords. He discovered leukoplakia, a typically benign condition characterized by white patches, in Weller’s larynx. The doctor told Weller he thought the patches looked suspicious for cancer and scheduled a biopsy.
The biopsy showed no cancer but did reveal signs of an airborne infection common in the Midwest called blastomycosis. The fungal infection, which can be caused by inhaling decaying leaves or soil, is often harmless. But some people, especially those with weakened immune systems, can develop flulike symptoms that are sometimes severe. Weller had been hauling bags of seeds in his car and soon afterward was short of breath.
The ENT prescribed a potent antifungal drug to knock out the infection.
It didn’t help. A week later, Weller experienced a severe sore throat. The doctor prescribed azithromycin, an antibiotic, for a possible strep infection.
Still no better, Weller was referred to a second otolaryngologist, who sent him to an infectious-disease specialist, who in turn advised that he see a gastroenterologist. Other than suspected blastomycosis, nothing was found.
With the help of his wife, a veteran nurse, Weller tried to coordinate care with his family physician. That was hard, he said. The doctor was ill and her group practice seemed severely overloaded.
“They would often cancel appointments at the last minute," Weller recalled. "I was very frustrated.”
Other than prescribing more drugs, some of which made him feel worse, no doctor seemed to know what might be causing Weller’s proliferating symptoms.
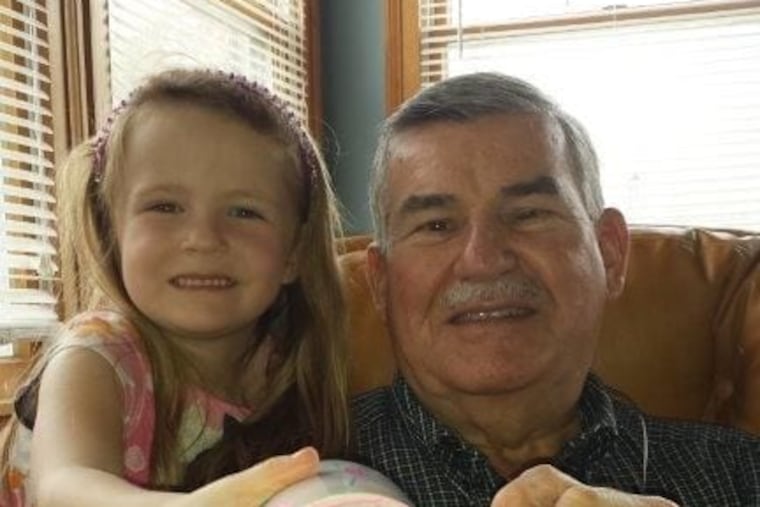
In November 2017, Weller had an unsettling incident at an Italian restaurant while celebrating his oldest granddaughter’s 18th birthday.
A few bites into his favorite short ribs, he felt a wave of fatigue engulf his jaw. Chewing became laborious. Swallowing was an impossibility. Weller surreptitiously spit food into his napkin, relieved to see the others weren’t paying attention to him.
A week later, Weller saw his primary-care doctor. His ability to chew and swallow had returned, although he could consume only soft food. And if he wasn’t careful, he would choke, sometimes aspirating what he was eating.
His fatigue had worsened to the point that he was unable to walk across his average-sized yard without stopping several times to rest. And his gait was off: When he walked, Weller said, his feet flapped. His doctor ordered a chemical stress test and an echocardiogram.
“The cardiologist told me it’s not your heart — it’s fine,” Weller recalled. “You’re going to have to look elsewhere.”
Feeling increasingly desperate, Weller decided to see what he could unearth online.
Solution
While taking azithromycin for possible strep, Weller had read the warning label. It cautioned that the drug should not be taken by people who have myasthenia gravis because it can aggravate the disorder. Weller had never heard of myasthenia gravis (MG), a chronic neuromuscular autoimmune disorder that causes weakness in the muscles responsible for breathing and movement. But he had felt dramatically worse after taking the drug — and it turned out he hadn’t even had strep.
His search led him to the Mayo Clinic website and a description of symptoms that sounded awfully familiar: muscle weakness, fatigue, shortness of breath, difficulty chewing and swallowing, and gait disturbances. Symptoms typically improve with rest.
Weller discovered that he had nearly every MG symptom listed except the most common: double vision and droopy eyelids known as ptosis. The disorder, caused by a transmission error between nerves and muscles, can be diagnosed through a blood test. The test measures the level of an antibody that disrupts normal communication at the neuromuscular junction — the place where nerve cells connect with the muscles they control.
Weller called the Mayo Clinic but was unable to wrangle an appointment with the neurology department in Rochester, Minn., so he decided to see what he could accomplish locally.
He was scheduled to see his family doctor in mid-December, but the appointment was canceled at the last minute. He arranged instead to see a nurse practitioner. Then he compiled a list of symptoms — numbering more than a dozen — along with a page of questions. His goal was to get a blood test used in the diagnosis of MG.
His strategy worked. The nurse practitioner ordered a test for acetylcholine receptor antibodies, which can help distinguish MG from other neuromuscular disorders.
“I really credit her with listening and doing what I asked,” Weller said.
Five days later, Weller learned that his hunch was correct.
His AChR antibody level was roughly 1,200 times higher than normal. He had MG, which affects about 20 per 100,000 people in the United States.
“I’m very confident a neurologist would have recognized this,” said James B. Caress, a professor of neurology at Wake Forest School of Medicine in Winston-Salem, N.C., who specializes in treating MG. (Weller’s neurologist and primary-care doctor declined to be interviewed.)
Difficulty chewing, Caress said, is a classic sign of the disorder, which killed Aristotle Onassis in 1975, before treatment had improved. It’s possible that a family physician, especially one practicing in a small metropolitan area — the Bloomington region has a population of about 168,000 — might never have seen a case, he added.
Caress speculated that doctors might have been misled by the fungal infection.
Whether Weller actually had blastomycosis is unclear. No confirmatory test was performed, Weller said.
Weller and his wife were in Louisiana visiting their daughter when he learned the result of the antibody test. The couple drove home a few days before Christmas, but a few hours after starting the 720-mile trip Weller’s right eyelid suddenly drooped shut. It was his first experience with ptosis.
“That was the low point,” he said.
A neurologist in Peoria determined that Weller had a severe case of MG and was at risk for one of the most feared complications of the disorder: a breathing crisis that occurs because the muscles that control respiration become too weak to function. A crisis can require emergency treatment including a ventilator.
Weller immediately began taking prednisone, a corticosteroid that suppresses the production of antibodies, along with other medicines.
For the last year he has undergone plasmapheresis every other week. The treatment, which filters the blood in a manner similar to dialysis, removes antibodies, but its effects wear off quickly.
Weller said he feels confident in his neurologist, who is treating several other people with MG.
In the last two months, his health has deteriorated for reasons that aren’t clear. “It’s a roller coaster,” he said. “I get up, take my meds, and see how I am today.”
Weller wishes he’d pushed for an explanation of his prolonged hoarseness and other symptoms much sooner.
“I would tell people to pay attention to what’s going on,” Weller said. “Nobody knows your body better than you.”