FDA approves second breakthrough therapy for sickle cell disease in less than a month
For the first time, sickle cell patients have a drug that treats the underlying cause of the disease
For the 100,000 Americans with sickle cell disease, their families, and their clinicians, this is an unprecedented time of optimism.
The U.S. Food and Drug Administration this week gave accelerated approval to Global Blood Therapeutics’ Oxbryta (voxelotor), a novel drug that treats the underlying cause of the disease by boosting hemoglobin, the oxygen-carrying molecule in red blood cells.
The agency’s endorsement came three months earlier than expected — and just 10 days after it approved Novartis’ drug Adakveo, which has been shown to dramatically reduce sickle cell pain crises by making cells less sticky.
“This is truly an exciting time for sickle cell disease,” said pediatric hematologist Kim Smith-Whitley, director of the comprehensive sickle cell center at Children’s Hospital of Philadelphia. “These two new agents address different pathways, so we hope there will be synergy.”
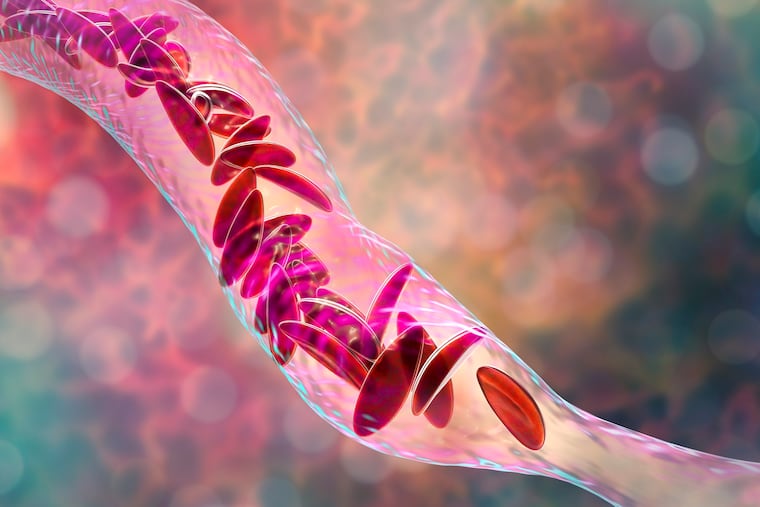
Sickle cell disease, an inherited disorder that primarily affects African Americans, is caused by a mutation in the hemoglobin gene. The abnormal hemoglobin is oxygen deficient, which causes red blood cells to become rigid, sticky, and crescent-shaped. These misshapen cells can hook together and block blood vessels, triggering excruciating pain and cutting off oxygen to vital organs.
Hydroxyurea, developed as a cancer drug, was approved for sickle cell in 1998 because it increases hemoglobin in red blood cells. The only other approved drug until now was Endari, approved in 2016 to reduce oxidative stress on deformed cells.
Oxbryta works by keeping hemoglobin more oxygenated, thus helping the red blood cells stay round and mobile. In the clinical trial that led to approval, 51% of patients on a high dose of Oxbryta had a significant increase in hemoglobin, compared to 6.5% on placebo.
“With Oxbryta, sickle cells are less likely to bind together and form the sickle shape,” Richard Pazdur, a director in the FDA’s center for drug evaluation and research, said in a news release. “This therapy provides a new treatment option for patients with the life-threatening disease.”
“After decades of waiting, we now have a treatment option that could change the course of this disease," Beverley Francis-Gibson, president and CEO of the Sickle Cell Disease Association of America, said in Global Blood’s news release.
Despite the way Oxbryta works, it did not significantly reduce the frequency of pain crises, or improve patients’ assessments of their qualify of life, in the pivotal clinical trial, published this year in the New England Journal of Medicine.
“I think the verdict is still out on how much it will improve fatigue, pain,” and dangerous respiratory problems, said Smith-Whitley.
However, she added, researchers hope Oxbryta will reduce patients’ risk of stroke and their need for blood transfusions, which can lead to dire complications.
The new drugs come as dozens of experimental therapies are in development, including some genetically engineered treatments that may offer a cure by repairing hemoglobin’s ability to carry oxygen. Early this year, for example, the FDA gave “fast track designation” to Vertex Pharmaceuticals’ gene-edited stem cell therapy for the disease.
Global Blood said its once-daily pill, which can be prescribed to patients 12 and older, will cost $125,000 a year before discounts. Novartis has priced Adakveo, a monthly intravenous infusion for patients over 15, at an annual cost of $84,000 to $133,000, depending on the patient’s weight.
Smith-Whitley said that while price “is a barrier, unfortunately,” the sickle cell community — including patients, advocates, and clinicians — has been meeting with drug makers and insurers to try to ensure patients’ access.