Q&A: How do I know if I’m having a ‘silent’ heart attack?
Some people don’t experience the classic symptoms of a heart attack, or don’t experience them as severely. This is known as an atypical presentation, or “silent” heart attack.
Q: How do I know if I’m having a ‘silent’ heart attack?
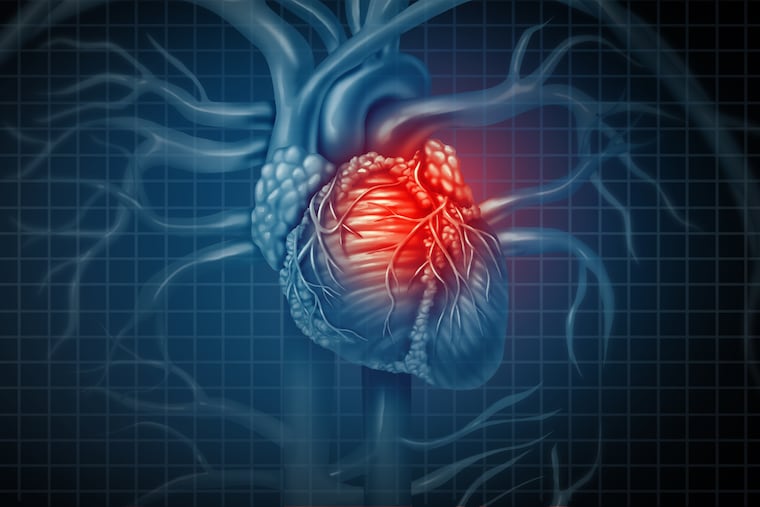
A: When someone experiences a heart attack, plaque builds up inside the blood vessels to the heart and blocks blood flow to the heart. When that happens, the heart tissue loses its source of oxygen and starts to die.
Many know about the classic symptoms of a heart attack, also called a myocardial infarction: pain or heaviness on the left side of the chest. This pain may radiate to the jaw or left arm, and be accompanied by other symptoms such as nausea, vomiting, shortness of breath, or extreme sweating.
But some people don’t experience these symptoms, or don’t experience them as severely. This is known as an atypical presentation, or “silent” heart attack. Because these symptoms are harder to detect, they are often mistaken for less severe issues such as nausea or heartburn or a flu-like feeling of aching muscles.
“Silent” heart attacks may not be as severe as a larger coronary event, but they can lead to one through continued damage to arteries and thickening of the heart walls — called cardiomyopathy — over a long period of time.
Because “silent” heart attacks generally lack warning signs, people who are at risk for heart disease — smokers, those with diabetes or obesity, or those with high cholesterol or family histories of heart disease — should talk with their doctor about their blood pressure and cholesterol levels and ensure regular exercise to decrease their risk. (Women are also more at risk for these types of episodes, although it’s unclear why. )
To diagnose the issue, your physician may recommend tests such as an electrocardiogram (ECG) to look for signs of poor blood flow, or an echocardiogram (echo test) — an ultrasound that shows the heart’s valves and chambers so your physician can see how your heart is functioning. Abnormalities on these tests may lead to further evaluations.
Erik Polan, DO, is an internal-medicine physician at Philadelphia College of Osteopathic Medicine.