Temple researchers eliminate HIV in infected mice
A novel therapeutic approach effectively cured HIV infection — in mice.
Temple University researchers on Tuesday said they had combined an experimental long-acting HIV therapy with a gene-editing technique to eliminate the virus from the genetic code of about one-third of treated mice.
The study, published online in the journal Nature Communications, was done in collaboration with University of Nebraska Medical Center researchers, who are developing a long-acting, slow-release version of current antiretroviral therapy. The experimental drug could enable once-a-month HIV treatment, which could improve patients’ adherence to the drug regimen.
While two-thirds of the treated mice still had some latent infection, the researchers said the study was the first to eradicate the AIDS-linked virus in living animals. The feat is an important step toward a possible cure for HIV infection, the researchers said.
A cure for HIV has been elusive because the virus can maintain hidden reservoirs of infection in the brain, bone marrow, spleen, and other organs. Antiviral drugs suppress HIV replication so that only a fraction of immune cells have the infection, but if the drugs are stopped, the latent virus can break out and resume destroying the immune system.
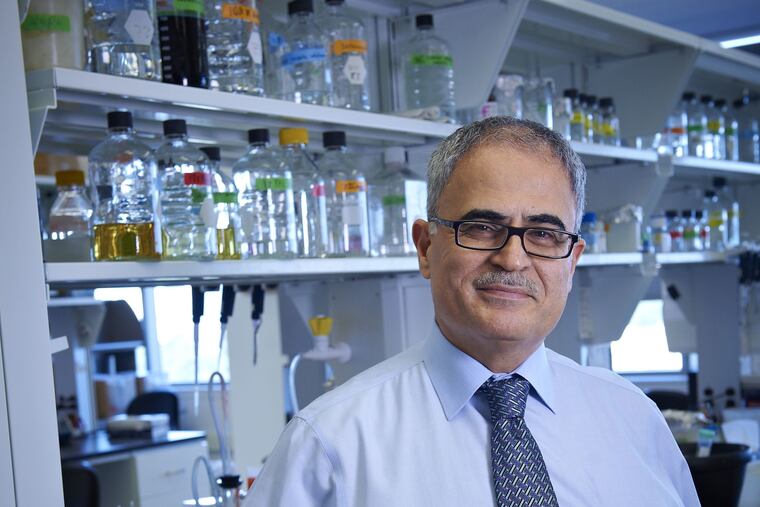
Kamel Khalili, chair of Temple’s department of neuroscience and a senior investigator of the new study, has spent five years using the gene-editing technology CRISPR-Cas9 to shut down HIV replication by snipping out large fragments of viral DNA from infected animals’ cells.
But like antiviral drugs, gene editing has proven insufficient to eliminate latent HIV.
For the new study, Khalili joined forces with a scientist he has known for 25 years — Howard Gendelman, an infectious disease and pharmacology researcher at the University of Nebraska. The long-acting HIV therapy being developed by Gendelman’s team targets viral reservoirs and suppresses HIV replication for extended periods with a single dose. The drug is packaged into nanocrystals that slowly release it over weeks.
“We wanted to see whether [the long-acting drug] could suppress HIV replication long enough for CRISPR-Cas9 to completely rid cells of viral DNA,” Khalili said.
The ability to precisely edit genes is seen as a potentially revolutionary medical tool, but CRISPR technology is barely eight years old, and continues to face technical and ethical obstacles. Late last year, the University of Pennsylvania launched the first U.S. trial in humans, using CRISPR to engineer immune cells to fight certain cancers. Several other human trials have since been approved in the U.S.
Khalili said the next step in the HIV research is to optimize the combination of virus suppression and gene editing, then try to use it in nonhuman primates, specifically monkeys. He is also scheduled to talk to the U.S. Food and Drug Administration about testing the approach in human clinical studies.