Philadelphia has a rich history of vaccine research and development
They're now luminaries of medical textbooks, but in the 1980s, Paul Offit and Fred Clark were in a Philadelphia lab, elbow-deep in stool samples collected from calves with diarrhea.
They’re now luminaries of medical textbooks, but in the 1980s, Paul Offit and Fred Clark were in a Philadelphia lab, elbow-deep in stool samples collected from calves with diarrhea.
They were on a mission to develop a vaccine for rotavirus, a deadly disease that filled the hospital beds of pediatric wards, claiming many lives.
Without a vaccine, in the first five years of life, four in five children would have symptoms of a viral infection, one in seven would wind up in the ER, and one in 200,000 would die from the disease, according to the Centers for Disease Control and Prevention.
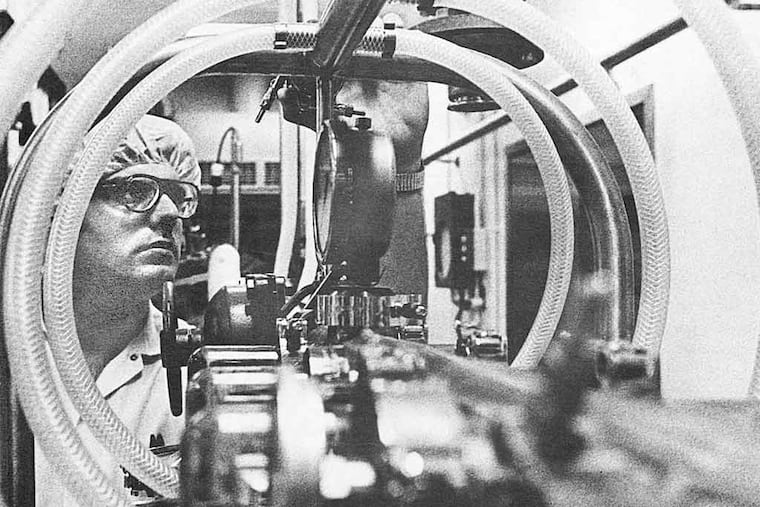
Under the guidance of Philadelphia vaccine guru Stanley Plotkin, Clark, a veterinarian, and Offit, a pediatrician, used cells growing in petri dishes to purify rotavirus strains from the sick calves. Combining those strains with human genes to create what is known as a reassortant vaccine, the product, Offit said recently, "retained the weakened virulence characteristics of the animal strain but also included the human genes that induced an immune response."
Their collaboration, spanning 26 years, multiple disciplines, and three institutions - the University of Pennsylvania, the Wistar Institute, and Children's Hospital of Philadelphia - was ultimately successful. In February 2006, the culmination of their hard work won FDA approval, propelling their vaccine onto the market.
"Now, the virus is virtually gone," Offit said. "It works and appears to be safe."
Philadelphia's rich history of vaccine development stretches back to the 1960s, and many of its highlights came under the direction of leaders from Penn's Perelman School of Medicine, this year celebrating its 250th anniversary.
Maurice Hilleman, a Merck & Co. Inc. researcher known in virology circles as the founder of modern vaccines, was stumped.
It was 1963. He was already well on his way to developing a vaccine for mumps, but measles was also raging. From 1958 to 1962, an average of about 500,000 measles cases were reported each year in the U.S., with nearly 500 associated deaths, according to the CDC.
A vaccine was in the works at Boston Children's Hospital, but as the scientists soon found out, it was toxic. Hilleman needed to figure out a way to make the new vaccine safe. And he needed to do it quickly before the disease claimed more lives.
He reached out to Joseph Stokes Jr., a professor of pediatrics at Penn, who proved to be a linchpin in the project.
Stokes' expertise was immunity, specifically a substance made from blood plasma called gamma globulin, which contains antibodies. He thought gamma globulin might help the measles vaccine.
The men tested the Boston group's vaccine on infants born at a New Jersey women's prison: a shot of gamma globulin in one arm and a measles vaccine shot in the other. Sure enough, Stokes' idea greatly reduced the toxic side effects of the vaccine.
Hilleman soon figured out other ways to administer the measles vaccine without the need for two separate shots, but in the meantime, Stokes' contribution saved lives.
Around the same time Hilleman was struggling with the measles vaccine, Stanley Plotkin had his own challenges.
The pediatrician came to Wistar in the 1950s to work on an oral polio vaccine with the renowned Hilary Koprowski. He also served on the faculties of CHOP and Penn.
In spring 1962, upon finishing his work with Koprowski, he went to London's Great Ormond Street Hospital for additional pediatric training. It was there that he saw the devastation of a rubella outbreak among pregnant women.
Baby after baby came under his care with symptoms of congenital rubella syndrome, or CRS: deafness, blindness, congenital heart disease.
He returned to Philadelphia in time to see the same pattern on this side of the Atlantic. In 1964 and 1965, there were 12.5 million cases of rubella, and 20,000 children in the U.S. were born with CRS.
The outbreak here was just as bad as he had experienced in London. Plotkin estimated that in Philadelphia, 1 percent of all babies born during that pandemic had been exposed to the virus.
"At that point, I was very interested in developing a vaccine," Plotkin, 83, said in a recent interview, "and set to work doing so."
Plotkin cultivated the viruses from a fetus that had been aborted by a woman who had contracted rubella and feared the impact on her child. At the same time, researchers at Wistar were showing that human fetal cells might prove to be a good replacement for animal cells in vaccine development. Plotkin raced against two other groups - the FDA and a team in Belgium - to develop the safest vaccine possible in the least amount of time.
"By the late '60s, there were several candidate vaccines," Plotkin said. But he believed his was the safest.
"The cells in which [the virus] was grown were free of any contaminating agent," unlike the animal cells other groups used, he explained.
"The majority of people in the field were excited with the idea and practicality of using human cells to develop vaccines, but the licensing authorities were concerned about it."
Europe beat the U.S. in licensing Plotkin's rubella vaccine in 1972, with American regulators following suit in 1979. Today, Plotkin's rubella vaccine is the one that is combined with the measles and mumps vaccines to create the MMR II.
In the early 1970s, Robert Austrian, a Penn professor of research medicine, was studying pneumococcal infections, a serious bacterial invasion of the upper respiratory tract. Although antibiotics had been in lifesaving use for decades, Austrian found they didn't lessen the incidence of infection. There were still hundreds of deaths from pneumococcal pneumonia.
Even today, it is estimated that 900,000 Americans will get pneumococcal pneumonia each year and that up to 7 percent of them will die from it.
Austrian knew prevention was essential.
In his lab, he set out to identify the number and type of disease-causing pneumococcal bacteria strains. His results suggested that 14 strains accounted for much of the disease and that all of them needed to be in a vaccine if it were to be effective.
Austrian worked with Hilleman at Merck on manufacturing the vaccine, which was licensed in 1977. The duo followed that up in 1983 with a pneumococcal vaccine that protected against 23 strains - the most complex vaccine ever developed.
Today, Penn remains a driving force in the field of vaccines. Now, the target is cancer.
"From history," said Robert Vonderheide, vice chief of research in the hematology-oncology division of Penn's Abramson Cancer Center, "the most important lesson we've learned is that you must vaccinate the individual before they are exposed to the pathogen."
His group is working to create a vaccine that could prevent malignancies from forming in healthy individuals who are at heightened risk for developing cancer. The vaccine is being tested on patients in remission from breast, lung, or pancreatic cancer with a high risk of relapse, but the hope is that the vaccine will prevent nearly every type of tumor from forming, Vonderheide said.
"It's a gene-therapy vaccine," he said, "and we're testing it for the first time for patients in remission from their cancer."
Phase-one clinical trials are underway in collaboration with another Philadelphia-area pharmaceutical company, Inovio.
“People thought it would be impossible,” Vonderheide said. “But based on science and based on new research, it might be within our grasp.”