Pennsylvania prisons face a deadly ‘full-blown resurgence’ of COVID-19
By Nov. 11, the number of positive cases reported by the department stood at 442 prisoners and 244 staff.
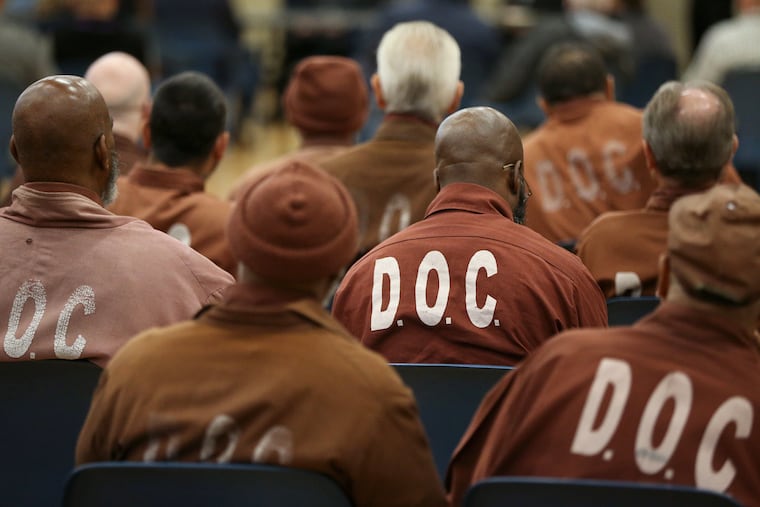
As the coronavirus shut down Pennsylvania in March, state prisons slammed into lockdown. Prisoners got 45 minutes a day for showers, phone calls, and fresh air — and spent the other 23 hours and change in their cells, waiting out the pandemic.
It seemed to work: By late May, there had been fewer than 160 confirmed COVID-19 cases among state prisoners. The Pennsylvania Department of Corrections' strategy was lauded as one of the most successful in the country, and some restrictions there were relaxed over the summer.
Now, though, advocates and prisoners are ringing alarm bells about outbreaks in institutions across the state — and about a potentially dire situation at county jails where local administrators are releasing little, if any, information about infections.
“What we’re seeing is a full-blown resurgence of coronavirus across Pennsylvania and it’s being seen in Pennsylvania state prisons,” said Claire Shubik-Richards, executive director of the Pennsylvania Prison Society, a nonprofit that advocates for humane conditions. So far, 17 incarcerated people have died — six of them since mid-October, at six institutions around the state. By this week, the number of positive cases reported by the department stood at 442 prisoners and 244 staff. “Twenty-one of the 23 state prisons have active cases. There has not been a single time during this pandemic that there have been that many active cases.”
And though public-health experts have urged “widespread and continuous” testing of workers and prisoners, Pennsylvania Corrections Secretary John Wetzel has emphasized a different approach involving small cohorts, frequent cleaning, and lockdowns to control transmission.
A DOC spokesperson said testing is conducted on newly committed prisoners, “select vulnerable groups,” and those experiencing flulike symptoms. As for staff, “we provide tests for staff, but they must request it. We cannot mandatorily test employees.”
When staff have been tested, they have been coming back positive more than half the time, a review of test results reported by the DOC for the month ended Nov. 10 shows.
» READ MORE: COVID-19 outbreak infecting hundreds at Fort Dix is ‘escalating crisis,’ N.J. senators warn
The Centers for Disease Control and Prevention and the Equal Employment Opportunity Commission have said employers may require staff to undergo periodic viral testing, as long as it is “job related and consistent with business necessity.” The CDC in August recommended mass testing in prisons as a way to assess spread and control transmission — an approach echoed by Johns Hopkins University public health experts in guidelines published in October.
Testing for prisoners is also limited even at institutions with sprawling outbreaks. At the State Correctional Institution Chester, a few miles outside Philadelphia, 136 prisoners and 57 staff now have COVID-19, according to the DOC. In the month ended Nov. 10, around half of prisoners' test results and close to 90% of staff tests there were positive.
Omar Hooks, who is incarcerated at Chester, said he grew alarmed when the prison passed out power-of-attorney and property-release forms. A friend of his died after nearly half a century in prison. “This became far worse than anyone expected."
Another prisoner there, Dave Disciullo, said he and his cellmate both developed classic COVID-19 symptoms: cough, difficulty breathing, a loss of taste and smell, body aches, and lethargy. “If you didn’t have a fever or a temperature, you didn’t get tested,” he said. It seemed as if everyone on his cell block was sick, but only those with fevers were taken to get tested and placed in quarantine, either in the gym or the restricted housing unit, a space normally used for punitive solitary confinement.
» READ MORE: Pa. prisoners are locked in their cells 23 hours a day. This is what it’s like, in their own words. (from May)
Hooks and others said many who are sick are not reporting it, given the dire conditions of quarantine. “The 14 days without shower, phone, etc. deters people who are sick from coming forward,” he said.
For Disciullo, the frustration is not only did he endure COVID-19, but his cell block is still on “enhanced” lockdown. “Every two days we get out for 30 minutes to use the phone and get showers. I haven’t been outside in over 45 days.”
At the State Correctional Institution Dallas, 67 prisoners and 37 staff have tested positive in the last month, and one prisoner has died. “It personally scared me, and has caused me to pray more,” said Tyreem Rivers, who’s incarcerated at Dallas.
The DOC in recent months began testing wastewater at the prisons. After detecting elevated virus levels in sewage at SCI Laurel Highlands, which houses geriatric and medically frail prisoners, it conducted its first round of mass testing there. According to the DOC, just 3% of prisoners tested positive.
Joseph Amon, a Drexel University professor and director of the university’s Office of Global Health, was skeptical of that approach.
A high concentration of the virus in sewage, he said, “is going to be a signal that occurs after the fact. You’re going to see this after people are infected," he said. “My expectation is doing more broad-based regular testing would help identify where the outbreak is centered, who are the closest contacts.”
The spread in state prisons mirrors trends across Pennsylvania, where COVID-19 infections have reached record highs.
Meanwhile, in Philadelphia, 80 prisoners and eight staff tested positive at the Federal Detention Center, U.S. attorneys wrote in a recent court filing.
Shubik-Richards, the Pennsylvania Prison Society director, said it’s unclear how many in county jails statewide are infected.
“We don’t know, because our county governments aren’t telling us, and that is astounding,” she said. “We have been encouraging counties to do rapid testing of staff as they’re required to do for their nursing homes. We don’t know if they’re using the testing on staff.”
» READ MORE: Lawsuit over Philly jails’ pandemic response alleges grim conditions, 24-hour lockdowns
A city spokesperson declined to answer questions about active cases in Philadelphia’s county prisons. In recent court filings, the city reported that units in every facility have been placed under quarantine in October or November due to possible exposures, and six prisoners have tested positive in the last week.
Advocates, who sued the city in federal court in April, say the city needs to do much more to keep prisoners and staff safe.
Five months after the jails agreed to a monitoring protocol, prisoners who submitted affidavits in the case still report limited access to soap, cleaning supplies, or even running water. Many report having only one or two paper masks to use for months. One woman said that when her mask became damaged, she was denied a new one and was not allowed out of her cell at all.
Philadelphia County prisoners have been on lockdown that entire time, allotted 45 minutes out of cell. But many say they often go days without that 45-minute break. Some allege that their signatures were forged on paperwork showing otherwise.
Su Ming Yeh, executive director of the Pennsylvania Institutional Law Project, is urging widespread testing, as well as access to the supplies prisoners need to protect themselves from disease.
“I very much fear for the incarcerated people in the Department of Prisons, and for their health and safety,” she said. “Despite some marginal improvements, overall there are still systemic issues which are highlighted by the increased numbers of COVID-19 in the community. It increases the risk for everyone.”