Temple doc among global leaders in COPD research
On Wednesday, international experts on a devastating lung disease will gather in Philadelphia to discuss the latest research on prevention and treatment.
On Wednesday, international experts on a devastating lung disease will gather in Philadelphia to discuss the latest research on prevention and treatment.
Chronic obstructive pulmonary disease, better known as COPD, is the third leading cause of death in the United States, according to the American Lung Association.
The meeting is part of a global initiative to raise awareness about COPD, heighten prevention efforts, promote better treatments, and improve outcomes for those who have it.
Despite how common the condition is, there is still much to learn. For example, long-term oxygen therapy has been a standard treatment for patients with severely low blood-oxygen levels. A long-standing question has been whether oxygen therapy would also benefit those whose levels are a bit higher. In a study published recently in the New England Journal of Medicine, researchers at Temple University and other centers found that it neither improved survival or reduced hospitalizations for these patients. The study was funded by the National Institutes of Health and Medicare.
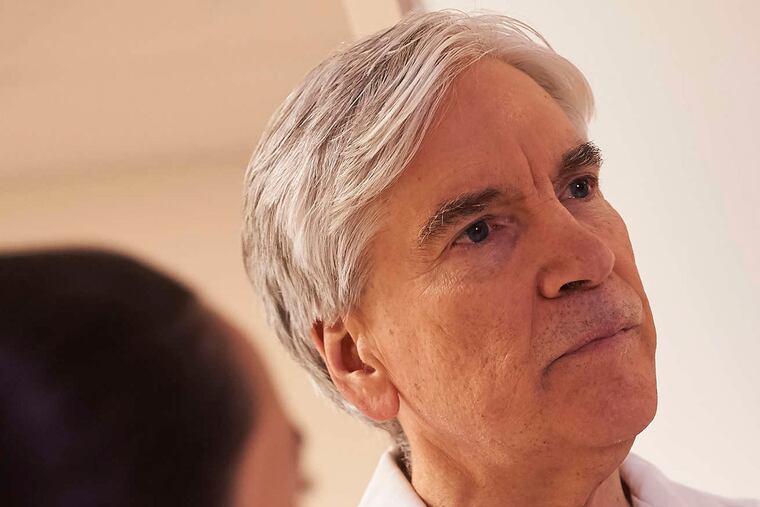
The Temple portion of the study was led by Gerard Criner, chair of the department of thoracic medicine and surgery at the Lewis Katz School of Medicine. Criner also is the director of Wednesday's conference.
He spoke to us recently about COPD.
What causes COPD? How many people have it?
About 90 percent of cases are related to cigarette smoking, but there are other things that contribute. These include childhood asthma, childhood respiratory infections, poor lung development, occupational exposures. All people who develop this disease have different trajectories for arriving at chronic air flow obstruction, which is the sine qua non of COPD. Some have normal lung function and then smoke. Some have an occupational exposure and lose lung function. Others have poor lung growth, either from asthma or from other factors we don't know.
One patient dies from COPD every four minutes - about 150,000 to 160,000 deaths per year. About 12 million people in the U.S. have been diagnosed with COPD, but we estimate that the disease is underdiagnosed by 50 percent.
What is life like for people with COPD?
They are breathless, mainly with exertion. But when it advances, they are breathless at rest. There are episodes that are escalations of their chronic symptoms of cough, mucus and fatigue. These can be related to environmental changes - the changing seasons, or times when air quality is bad. Patients can have flare-ups with viral or bacterial infections.
What does some of the latest research show?
We used to think there wasn't much we could do for this disease, but we now know this isn't true. A lot of different therapies have been developed, and fortunately the number of therapies is increasing drastically.
In the past year, multiple publications have looked at things like the endobronchial valve, a small device that is implanted in the airway. The valves block the air from going into a part of the lung and, instead, let it come out. Imagine that a part of your lung functions like a big distended balloon that won't deflate. If you take a big breath and let a little out and then try to take another breath, it's harder. But if you could empty the balloon with these devices, that will help the person breathe better.
Another example is that for people who are more prone to flare-ups, there are now a variety of medications that can be used to reduce their risk by providing better lung function or reducing inflammation. Recent research has shown the potential for using preventive therapies such as inhalers, antibiotics or other drugs.
Oxygen therapy is beneficial for some patients, but as the study published last month showed, not all.
Rehabilitation is another new area. Exercise doesn't make the lung stronger, but it makes the rest of the body stronger.
We also know now that comorbidities are prevalent. People who have COPD often also have diabetes or hypertension or sleep apnea or asthma. If we look at them all together, we can treat people in a more holistic way and make patients' lives better.
Why is Wednesday's event important?
This global initiative, close to 25 years old now, was started by the National Institutes of Health and major international respiratory societies to bring awareness to COPD, to escalate research and treatment and to give some uniformity to care across the world. It's the deliberations of this nonprofit that look at all the important data for all stages of the disease, from assessment to diagnosis to treatment.
A report is published worldwide and is updated every year. But this year, we are releasing the first major revision since 2011. The event in Philadelphia will be the public announcement of the new revisions. The report will be simultaneously published in four major international journals.
What would you say to people with COPD?
I've been doing this for 33 years, and the research has moved faster in the last three to five years than it's ever moved. Although, if you talked to any COPD patient, that's not fast enough.
There's still no cure. That should be foremost in everyone's mind at the moment. We know the best prevention is to not smoke or to stop smoking. But trying to reverse the lung abnormality? That doesn't exist now.
A lot of people I see have gone through a couple different doctors and have been told there's nothing they can do. No patient should ever be told that by anyone, regardless. There's always something you can do to improve a patient's outcome. People should know that there are many things that could be done, and they should seek help to improve their outcome and to achieve their goals of improved care.