Ads for fancy adult diapers might make you think incontinence is normal. It’s not.
Even young women, especially those who've had a baby, can face problems with leaking. But doctors say no one should just accept incontinence, since there are good treatments.
It's hard to miss the fact that urinary incontinence is no longer a taboo topic — at least in the world of advertising.
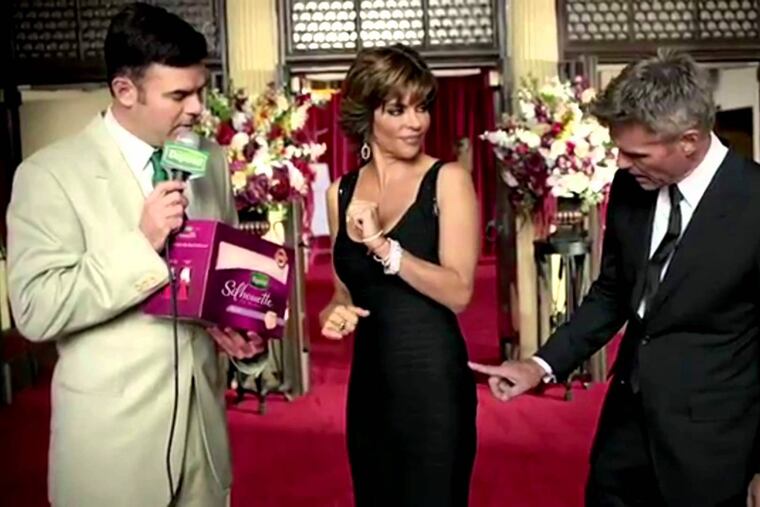
Print and TV ads abound featuring happy, middle-aged women dancing and laughing — two common triggers of embarrassing leaks — while wearing body-hugging versions of what once were called adult diapers. If you search the web, you can find sleek or lacy padded underwear, even thongs, designed to allow the millions of women who suffer from incontinence to feel sexy as well as secure.
Perhaps all that advertising for an industry that market researcher Euromonitor says topped $2 billion in the United States last year is helping women talk more openly about a common, often hidden source of shame. But does this marketing normalize a condition that is, in fact, not normal? Do the ads encourage women to settle for a lifetime of padding when good treatments are available?
Incontinence experts said innovative padding serves a useful purpose, and the ads have helped bring incontinence out of the shadows. But some worry that the advertising leads women to believe that incontinence is inevitable after a baby or two, or after menopause. They say women still wait too long to consult their doctors.
Common but not normal
Incontinence is "common in women, but that doesn't mean it's normal," said Tamara Bavendam, a urologist who is a program director of the division of kidney, urologic, and hematologic diseases at the National Institute of Diabetes and Digestive and Kidney Diseases. "One of the down sides of products is they can normalize it and, in the absence of any other information, it can allow women to think, 'I can hide this problem and I can go about my life.' "
>> READ MORE: There's another kind of incontinence and it's even more embarrassing
Alayne Markland, a geriatrician at the University of Alabama-Birmingham who has studied risk factors for incontinence, has similar concerns. Women with incontinence, she said, "often just don't seek care. They think there's nothing to do. … 'I'm watching all these ads about pads. That's what I have to do.' "
Anne Manning, a 37-year-old Philadelphia mother of 6-year-old twin sons and a 2-year-old daughter, said that after the birth of her twins, she started leaking when she would go running. She was "somewhat comforted" by ads for incontinence products. "I felt like, oh well, this is just life."
Eventually, she told her gynecologist, who sent her to another gynecologist, who sent her to Pia Leone, a physical therapist at Jefferson Health who specializes in helping patients strengthen pelvic floor muscles. These muscles are essential for bladder control but can also be a factor in hip and back problems. Manning had no idea such help existed. "I can't believe I've lived six years not knowing that I could possibly fix this," she thought. She began therapy in April and can now run without wearing a pad.
Bavendam thinks that urinary incontinence is much more than a quality-of-life issue. Bladder problems may contribute to why obese patients won't exercise. They may be the unspoken reason that a heart patient doesn't take a prescribed diuretic. They may lead to social isolation, a risk factor for medical decline that is getting growing recognition. She thinks all primary-care doctors should ask patients about incontinence.
Bavendam's agency has held two medical meetings on incontinence in the last two years, and is funding research on bladder health.
The Women's Preventive Services Initiative recommended Aug. 13 in the Annals of Internal Medicine that all women be screened for incontinence. The screening, the group said, should assess how incontinence is affecting quality of life. In an editorial, Australian researchers argued for a randomized trial measuring the value of such screening.
Incontinence is greatly underreported, Bavendam said, and also hard to define. Some women may leak a little a couple times a year. Others may leak several times a day. Women account for 80 percent to 85 percent of incontinence. Their risk rises with childbearing — Bavendam said the muscle trauma women endure with childbirth may be comparable to sports-related muscle damage — as well as with obesity, smoking, constipation, and age. Markland's study also found increased risk with asthma, high blood pressure, and high cholesterol. Men's incontinence also rises with age, but is often linked to prostate or neurological problems.
Long associated with age, incontinence is a common reason for nursing home placement. Yet an estimated 15 percent to 20 percent of women in their 20s and 30s have experienced incontinence, Bavendam said. By their 40s and 50s, 40 percent to 50 percent of women are dealing with it to some degree. Although some women may always need pads, experts said there are multiple treatment options.
"Cure happens, and a lot of people get a whole lot better," said Joshua Cohn, a urologist at Einstein Healthcare Network. "I try not to set people up for cure. I try to set people up for significant improvement in their quality of life."
Here’s how doctors treat incontinence
We spoke with Ariana Smith, a urologist at Penn Medicine, and Diane Newman, a nurse practitioner who co-directs Penn's Center for Continence and Pelvic Health; Michael Kennelly, director of the Charlotte Continence Center at Carolinas Medical Center and chair of the American Urological Association's bladder health committee; Mitchell Berger, a urogynecologist at Main Line Health; Cohn and Donald DeBrakeleer, urologists at Einstein, and Leone and Brandis Johnson, physical therapists who specialize in pelvic floor disorders at Jefferson Health.
They all said that getting a proper diagnosis is essential because treatments vary according to the type of incontinence. Stress incontinence leads to leakage when you cough or sneeze suddenly. Urge incontinence, which becomes more common after menopause, means a woman feels the need to urinate and can't hold it long enough to get to a bathroom. Some women have both types.
Bladder control involves a remarkably complex interplay between nerves and muscles, one that is taken for granted — until something goes wrong. For instance, although many people are worried about leaking urine, some have trouble fully emptying their bladders.
An adult woman's bladder can hold up to about two cups of urine. It's typical to require about eight trips a day to the bathroom, and you should be able to go two to four hours without needing to go. Most doctors don't get concerned about nighttime frequency unless you're up more than once or twice.
Strengthening the pelvic floor muscles, the muscles that span your crotch and support your inner organs, can help both stress and urge incontinence. These muscles support the urethra during sudden movements, such as laughing or bouncing, and can help women calm an overactive bladder. The pelvic floor can be damaged by pregnancy and childbirth or just grow weaker with time. The muscles are strengthened by Kegel exercises, a type of isometric movement that most women have heard about and, experts said, routinely do wrong.
"This is such a difficult muscle to isolate," Newman said. "We should be teaching women about this muscle prior to problems, prior to pregnancy."
Kegels aren’t easy
If you do Kegels right, you are squeezing and lifting the pelvic floor, a process you cannot see. If the muscles are weak, you can't feel it very well, either. Although some patients can figure it out on their own, doctors say it is often helpful to go to expert therapists who can provide biofeedback and go beyond Kegels to help women learn to coordinate the pelvic floor muscles.
Patients can also buy biofeedback devices that will help them do the exercises correctly at home. Newman likes Vibrance, which sells for $299. Leone suggests Elvie for $199 and kGoal for $149.
Physical therapy alone can help most women with stress incontinence. But once you start the exercises, it can take a few months to see results, and you have to keep doing them forever.
"When it comes to working out the pelvic floor, I don't think it's something women can do without a trainer," Cohn said.
Laura Wallace, 30, of Collegeville, became incontinent after the birth of her son two years ago and found it "really upsetting." She has found it challenging to fit in all the exercises that Newman wants her to do, but has also done an online pelvic floor program and joined a Pilates class. As for Kegels, she said, "I don't like them and I forget to do them." Wallace, who directs early learning at the Maternity Care Coalition, doesn't think post-partum health gets the attention it deserves. She wishes she'd been told more about pelvic floor health while she was pregnant.
Wallace, who is still getting physical therapy, said her muscles are stronger and the incontinence is "a lot better."
Women can also use an over-the-counter, tampon-like device that can support the urethra, but it's only a temporary fix. In the long run, Kennelly said, it's cheaper to buy a $60 prescription product that will last forever.
For muscle damage that exercise cannot fix, urologists can do several variations of a "sling" procedure, which uses tissue or mesh to support the urethra. It is 80 percent to 90 percent effective, Smith said.
The dysfunctional bladder
Urge incontinence can be more challenging than stress incontinence because it involves bladder dysfunction.
Feeling as if you need to urinate frequently can be a learned behavior. If you go a lot, the bladder learns to think it's full earlier. Many women can change that by gradually stretching the time between bathroom trips. Doctors also recommend that they keep diaries that show how often they're urinating and what they're eating. Bladder irritants can include coffee, tea, diet sodas, alcohol, and acidic and spicy foods. Ironically, drinking too little can make things worse by leading to concentrated urine, which is also a bladder irritant. On the other hand, many people drink too much. As long as your urine is clear, you're drinking enough, doctors said. Addressing constipation can also help. So can losing weight and quitting smoking.
Behavioral changes can help about a quarter of women with urge incontinence, Smith said. Another 25 percent to 30 percent may be helped by trying medication, either anticholinergics (which have been associated with cognitive problems) and newer, more expensive beta-3 agonists.
Many insurers require subscribers to try drugs before they can receive coverage for the next steps: Botox injections to relax the bladder and electrical stimulation. Patients can get a stimulator implanted or get outpatient stimulation through a nerve in the ankle.
Markland, the Birmingham geriatrician, hopes women will start talking more openly about incontinence and insist that something be done about it. "I really hope that baby boomers who are aging," she said, "are not going to put up with this."