Cancer questions over popular diabetes drugs raise furor
Newer diabetes drugs called “incretin mimetics” have clear benefits. But do they also raise the risk of pancreatic cancer? Amid uncertainty and legal controversy, patients are left with a dilemma.
Before he died early last year of pancreatic cancer, Stephen T. Johnson filed a lawsuit against Merck for not telling him his disease might be a side effect of taking Januvia, the company's blockbuster diabetes drug.
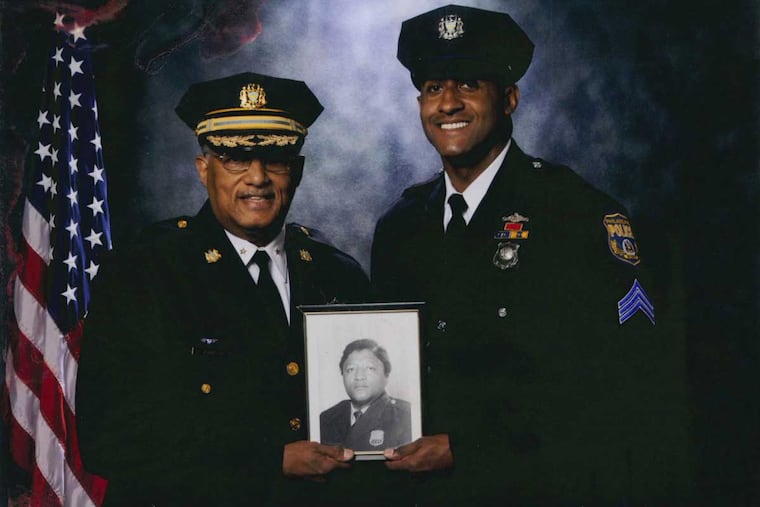
The 63-year-old Philadelphia police officer knew his life was at an end, but he wanted the product labeling changed to warn other diabetics.
"He worked his whole life. He didn't need the money," said his son, Stephen T. Johnson Jr., also a Philadelphia police officer. "But he felt it just wasn't right" that patients weren't informed.
A federal judge in California disagreed. In November, Judge Anthony Battaglia threw out more than 744 failure-to-warn lawsuits filed around the country against the makers of type 2 diabetes drugs known as incretin mimetics. He ruled that the companies, including Merck & Co., Eli Lilly & Co., and Novo Nordisk, were shielded from state court claims because the U.S. Food and Drug Administration would have refused to let them add pancreatic cancer to the labeling. The case is on appeal.
Soon after the ruling, the companies, worth a combined $4 billion, petitioned to collect $408,000 in legal expenses from the pancreatic cancer patients or their estates.
The plaintiffs' lawyers, including Max Kennerly in Philadelphia, are fighting back, saying the companies are not entitled to reimbursement and are just trying to scare off future litigants.
Meanwhile, the important question of whether incretin medications cause or contribute to pancreatic cancer remains unsettled, three years after the FDA announced an investigation. It is another example, critics say, of the limits of a regulatory system that relies on companies to ferret out the safety problems of their own products.
Diabetes has become a worldwide scourge, and use of incretin drugs - alone or in combination with other diabetes medications - is on the rise. In the United States alone, more than three million diabetics took the top five incretins in 2013, according to an estimate from the Institute for Safe Medication Practices in Horsham. Almost half of them took the top-seller, Merck's Januvia.
This drug group is growing - with nine approved compounds and counting - as are its possible uses. Incretins are in testing for Alzheimer's disease, polycystic ovary syndrome, heart failure, and reducing cocaine euphoria in addicts. Novo Nordisk's Victoza has already been approved, as Saxenda, for weight management in obese adults.
The FDA, the American Diabetes Association, the National Institute of Diabetes and Digestive and Kidney Diseases, many leading diabetes researchers - and all the drugmakers - say the evidence linking these drugs to pancreatic cancer is inconsistent and inconclusive.
"Nothing is more important to Merck than the safety of our medicines and the people who take them," Merck said in an email. "We will continue to vigorously monitor the safety of Januvia . . . in close collaboration with regulatory agencies and scientific experts."
But evidence of a link continues to accumulate.
Last month, a new analysis of the FDA's database of "adverse event" reports found pancreatic cancer developed at least 10 times more often in Januvia users than would be expected given the incidence of the disease. The cancer was also reported more often in users of AstraZeneca's Onglyza and Lilly's Tradjenta, according to the study, published in Annals of Pharmacotherapy.
Several previous analyses of the FDA database have also raised alarms. In 2013, the Institute for Safe Medication Practices concluded the odds of a report of pancreatic cancer were 20 times higher with patients on incretins than on other diabetes drugs.
"We recommend updating the prescribing information to include stronger alerts," wrote Thomas Moore, lead author of the institute's analysis.
Pancreatic cancer is rare, with about 12 diagnoses per 100,000 people a year in the U.S., federal data show.
That sets up a problem that plagues the drug-approval process: Even the largest clinical trials are too small to reveal rare side effects. The painkillers Vioxx and Bextra and cholesterol-lowering Baycol seemed safe until use by millions of consumers revealed deadly harms; all three were eventually withdrawn from the market.
Nonetheless, the FDA and many experts say manufacturers' clinical trials of incretin drugs are key to settling uncertainty over pancreatic cancer. So far, four studies the FDA mandated to assess cardiovascular safety have also looked for increased cancer risks - and found none. Another trial will soon present results; three are underway. In total, 138,000 patients will be studied.
Robert Ratner, chief scientific officer of the American Diabetes Association, said the results so far were reassuring and "even if there is a [pancreatic cancer] risk, it's extremely small."
But even a slightly elevated risk would add to a growing toll. Pancreatic cancer incidence is creeping up, even as the disease remains so difficult to detect and treat that only 4 percent of patients survive five years. The malignancy rose from the fourth-leading cause of cancer death to No. 3 last year.
Though the reason for the uptick in incidence is unclear, obesity and diabetes - the entangled epidemics of modern life - are risk factors for pancreatic cancer. That complicates the possible link between the cancer and incretins.
Since entering the U.S. market in 2005, incretin therapies have revolutionized diabetes treatment by mimicking natural human chemicals, called incretins, that increase secretion of insulin, the hormone that keeps blood sugar in check.
Unlike injected insulin and some other diabetes therapies, incretin agents don't lead to weight gain, or to the dangerous, sometimes fatal, drop in blood sugar called hypoglycemia.
Still, soon after the first incretin, Byetta, hit the market in 2005, the FDA began getting reports of users who developed dangerous inflammation of the pancreas, or pancreatitis.
As with pancreatic cancer, pancreatitis is a risk of diabetes, so teasing out drug effects is tough. But the agency noted that of 30 reported cases of pancreatitis, 22 patients improved after stopping Byetta.
In 2007, the FDA announced pancreatitis would be added to Byetta label warnings; a 2008 revision added pancreatitis that can cause hemorrhaging or tissue destruction.
All incretin therapies now carry the warning.
In 2009, endocrinologist Peter C. Butler, a respected diabetes researcher at the University of California, Los Angeles, began publishing a series of studies that turned him into a lightning rod in the safety debate.
Using animal models and pancreases from deceased human organ donors, Butler's group found that incretin therapy made certain pancreas cells multiply. This increased the weight of the organs. The therapy also seemed to fuel the growth of precancerous lesions, which were more common in incretin-treated pancreases.
Butler concluded that incretin therapy, while not triggering cancer, acted like a growth hormone.
Incretin treatment, "like estrogen in breast cancer, might promote development of pancreatic cancer in some individuals," he wrote in July 2013 in Diabetes Care.
He also called the emerging concerns "a familiar story: "A new class of antidiabetic agents is rushed to market and widely promoted. . . . Evidence of harm accumulates but is vigorously discounted. The regulators allow years to pass before they act. The manufacturers are expected - quite unrealistically - to monitor the safety of their own product."
Butler's methods and findings were harshly criticized. He stopped publishing on the issue, and he declined to be interviewed for this article.
In response to Butler's research using human pancreases, the FDA announced in March 2013 it was investigating reports of "precancerous cellular changes." Recommendations would be issued, the agency said, when its review was complete. Almost three years later, that announcement has not been updated.
However, two years ago, officials from the FDA and its European counterpart published a "perspective" in the New England Journal of Medicine. They said no firm evidence existed to link incretins to pancreatic injury - not even to pancreatitis, which is part of the label warnings - but the question remained open.
Meanwhile, a trickle of state lawsuits turned into a river after the FDA announced its 2013 investigation. Before they could proceed, Judge Battaglia was assigned to decide whether a warning about pancreatic cancer would have been impossible for the drug companies to add without violating FDA regulations.
In 2009, the Supreme Court ruled that even though drug-label changes require FDA approval, manufacturers bear primary responsibility for the information and can make label changes on their own to improve safety.
Battaglia nonetheless concluded the FDA would have rejected a pancreatic cancer reference if the drugmakers sought it - so the lawsuits were thrown out.
For Steven Johnson Jr., the unresolved debate stirs anguish. He remembers his father's efforts to control his diabetes so it wouldn't damage his eyes, kidneys, or feet.
"Here he was, trying to do the best thing for his health, and he gets something so much worse than diabetes," Johnson said.
215-854-2720@repopter