Genetic test helps pick the right drugs for mental health
Analysis of a simple cheek swab can guide the choice of drugs for depression, anxiety, and ADHD. Revenues at Genomind have more than doubled, from $6.2 million in 2014 to $13.1 million in 2016.
Like many people suffering from depression, Vince Sparks tried various drugs for decades with little long-term success.
In 2013, a genetic analysis, performed by a fast-growing King of Prussia-based company called Genomind, revealed a possible reason. The Mullica Hill resident was born with a genetic quirk that impaired his ability to convert folic acid into the form that is needed to metabolize the neurotransmitter serotonin. That meant drugs such as Prozac, a selective serotonin reuptake inhibitor (SSRI), provided little benefit.
Using those test results, an advanced-practice nurse told Sparks to take a supplement called L-methylfolate, the converted form of folic acid. That enabled him to start taking Prozac again, and he says the combination has allowed him to avoid sharp downturns in mood.
"I've been able to keep more at a stable level than I was before," said Sparks, 60, a freelance writer. "It certainly has helped."
Success stories such as his have helped drive the rapid growth of Genomind, where revenues more than doubled from $6.2 million in 2014 to $13.1 million in 2016. That placed it among the Philly 100 list of fastest-growing companies in the region, according to the Wharton Small Business Development Center. The number of employees has kept pace, as well, going from 39 to 81 during the same period — taking mental health into the realm of personalized medicine, long a part of cancer care.
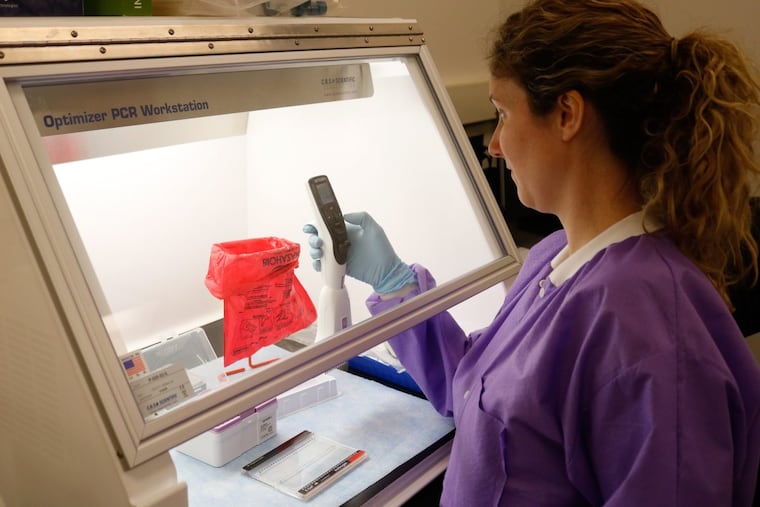
Every day at about 9:30 a.m., FedEx delivers 150 to 220 vials to the company's headquarters on Renaissance Boulevard, each containing a cheek swab from a patient seeking help in finding the right medication, said assistant laboratory director Betsy Bove.
The DNA in the samples is amplified and analyzed to detect the presence of specific variants in 18 genes. Six of them affect how the patient metabolizes medications in general, while the remaining 12 influence how a patient responds to drugs for specific mental-health conditions — including depression, anxiety, and attention-deficit hyperactivity disorder, said Dan Dowd, vice president of medical affairs.
The clinician gets the results in three to five days, guiding the choice of more than 20 classes of drugs and 122 individual medications.
The science behind the test is sound, said Michael E. Thase, professor of psychiatry at the University of Pennsylvania's Perelman School of Medicine. A key question for the company's future is how many insurance companies will decide it is cost-effective to pay for the test, in terms of helping patients to avoid hospital visits and other costly treatment.
Traditionally, when a drug does not work for a given patient, the mental-health provider simply prescribes a different one. But many such drugs take time to build up in the patient's system, so a trial of six weeks is common. In the meantime, there are not only increased medical costs, but depending on the type and severity of illness, there can be lost jobs, failed relationships, and suicide attempts, Thase said.
"If you go through three medications without benefit, you're talking about six months of your life," Thase said. "And bad things can happen in six months."
Some private insurers do not yet cover the genetic assay, called Genecept; those that do will pay up to $1,500, the company said. Private insurers generally expect patients to contribute up to $300, as well. Medicare pays only for testing certain genes for specific diagnoses, for a total of $400, the company said.
Hospital stays, on the other hand, typically cost thousands of dollars.
Clinicians in all 50 states have used the Genecept to guide treatment choices, and early evidence suggests it is having an impact.
In 2015, a company-funded study found that among more than 600 patients who underwent the Genecept assay, 62 percent reported clinically significant improvement in their symptoms. The success rate was even better among a subset of patients who had previously experienced at least two treatment failures. The study was not a randomized, controlled trial that researchers consider the "gold standard" for demonstrating efficacy, but such a study is now underway.
"At the heart of our company is a desire to find ways to try to help patients struggling with mental issues get better, faster," Genomind chief executive officer Michael Koffler said.
Genomind is not the only company taking this personalized approach to the field of mental health. Competitor Assurex Health, based in Mason, Ohio, also has seen rapid growth.
Sparks, who also takes a low dose of Xanax to treat anxiety, cautioned that faster identification of the right drug is not a panacea, as many patients also need therapy. But for him, genetic information was a valuable tool.
"It really pinpoints what is good for you on a genetic basis," he said. "You're not going to the doctor's as often. You're not having to make as many appointments because you finally found something that works for you."