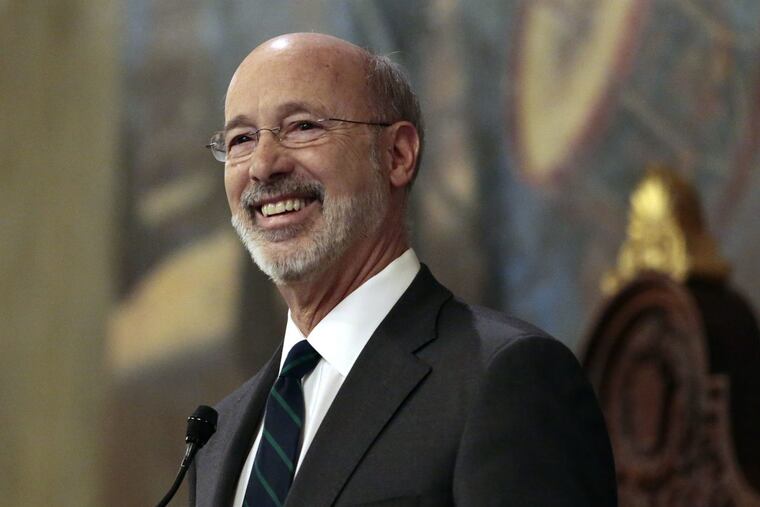
Gov. Wolf to announce Medicaid change aimed at opioid treatment
Pre-authorization can take up to 24 hours.
HARRISBURG — In an effort to help people get faster treatment for opioid addiction, the state will remove a pre-authorization requirement for Medicaid recipients prescribed some types of medication helpful for recovery, Gov. Wolf is expected to announce Thursday.
Pre-authorization can take up to 24 hours, and the administration hopes the change — which advocates have been calling for — will prevent situations where people struggling with addiction must decide whether to pay out of pocket for the medication, use drugs or risk going into painful withdrawal.
"If even one person is delayed access to the treatment they need, it is one person too many," Wolf, a Democrat, said in a statement. The governor will also ask private insurers to consider making similar changes, according to sources familiar with his plans. He does not have jurisdiction over Medicare, which runs through the federal government.
Wolf's announcement, expected Thursday afternoon at Crozer-Chester Medical Center in Chester, comes partway through a three-month long opioid disaster declaration, which allows government officials to temporarily suspend some regulations to help combat a deadly epidemic. But, this change will likely continue past the end of the declaration, according to two people familiar with the plan.
The waiver applies to medication-assisted treatments, such as Suboxone and Vivitrol, that help block effects of withdrawal or prevent people from experiencing a high. Patients often take those types of medications while receiving therapy or counseling.
Treatments like Suboxone and Vivitrol require a prescription from a doctor. They often also require a pre-authorization from insurance. The pre-authorization can come immediately, or it can take as long as 24 hours to process. With the waiver in place, a prescription alone will be enough to ensure that Medicaid recipients receive coverage for such treatments.
Groups that provide drug addiction services have been pushing insurers to remove pre-authorization requirements for medication-assisted treatment.
"That's going to save some lives," said Jose Benitez, executive director of Prevention Point. "We'll be able to prescribe much-needed medicine to people — it's a huge help."
Nationally, groups such as the American Medical Association have also advocated for the removal of pre-authorization requirements.
"When a patient seeking care for an opioid use disorder is forced to delay or interrupt ongoing treatment….there often is a negative impact on their care and health. With respect to opioid use disorders, that could mean relapse or death from overdose," the association wrote in a letter sent to attorneys general across the country.
Pennsylvania logged 4,642 drug-related overdose deaths in 2016, about 85 percent of which involved an opioid, according to an analysis by the federal Drug Enforcement Administration. Toxicology tests can take weeks to process, so numbers for 2017 are still being finalized, but state officials said they suspect there was an increase between 2016 and 2017.
Inquirer Reporter Aubrey Whelan contributed to this report.